Surgeon Interview: Dr. Jai Raman Discusses Minimally Invasive Heart Valve Treatment
By Adam Pick on June 26, 2010
Several weeks ago, I shared the touching story of William Luna’s high risk valve repair. Shortly thereafter, I received several emails about minimally-invasive procedures and Dr. Jai Raman — the surgeon who performed William’s procedure.
Given your interest in these topics, I contacted Dr. Jai Raman, Chief of Cardiac Surgery, at Rush Medical Center in Chicago, Illinois. Luckily, a few days later, I found myself chatting one-on-one with Dr. Raman. I thought you might like to read the highlights from our discussion:
Adam: Thanks so much for taking time to speak with me today. I’d like to ask you a couple questions about minimally invasive valve repair and replacement.
Dr. Jai Raman: Adam, it is good to talk to you and learn about the great service you provide to patients and caregivers.
Dr. Jai Raman: I moved here from Melbourne, Australia in July, 2002. I had helped develop and research some new procedures in the surgical treatment of heart failure and was attracted to the University of Chicago.
Adam: Can you estimate what percent of your operations require some form of valvular procedure?
Dr. Jai Raman: Approximately 60% of my cardiac surgery procedures involve some kind of valvular procedure.
Adam: Is there one valve that you find yourself operating on most?
Dr. Jai Raman: Aortic and mitral valves in equal numbers. Frequently though, there is another valve that also requires attention. For example, very often when we work on the mitral valve, the tricuspid valve also needs attention. Fortunately, we are blessed with a very dedicated and collaborative group of echocardiologists and anesthesiologists with echocardiographic expertise. We discuss all our prospective and interesting cases every week in a valve group meeting — that grew out of informal meetings between me and Dr. Sugeng, one of our expert echocardiologists.
Adam: Of all your valve work, can you estimate how often those procedures utilize a minimally invasive approach?
Dr. Jai Raman: Unless the patient has a definite contra-indication or needs bypass surgery, almost all valve surgery is performed through a minimally invasive approach. I believe I have developed the largest experience with this approach in the Chicago-land region.
Adam: Has the percentage of minimally invasive procedures increased over the past few years? If so, why?
Dr. Jai Raman: The percentage has definitely increased over the past few years. I first started using minimally invasive procedures in an effort to get trained to use the Da Vinci “robot”. For me, the “robot” is somewhat constraining in terms of set-up time, equipment and cannot typically be used in high-risk cases. I found that I could reduce risk of bleeding and major post-operative complications by adapting minimally invasive approaches to high-risk and redo cardiac surgery. As the learning curve has been overcome, I have become extremely comfortable using these techniques over the past 6 years, so that MICS (minimally invasive cardiac surgery) is the norm in my practice.
Adam: What do you feel are the key patient benefits for a minimally invasive procedure?
Dr. Jai Raman: Less pain, less bleeding, quicker recovery, better acceptance by the patient and the families. Don’t get me wrong, the sternotomy is a great incision and has helped us advance the frontiers of cardiac surgery. However, there is an obligatory amount of bleeding, pain, discomfort, delayed recovery, etc. that accompany this standard approach to most cardiac procedures.
Adam: From the surgeon’s perspective, are minimally invasive procedures more difficult considering there isn’t direct, open access to the heart?
Dr. Jai Raman: That is a great question, Adam. Definitely, MICS (Minimally Invasive Cardiac Surgery) requires a different mindset. We have to remember that our primary goal is to repair or improve the heart. The approach to the part of the heart that needs fixing can be tailored to minimize the amount of cutting and trauma. Except for transplantation — where the entire heart needs to be replaced — potentially most other cardiac procedures can be performed through less invasive approaches. However, it is vital that the surgeon and his/her team that perform these procedures are comfortable with that approach and are capable of handling complications that might arise. Unfortunately, I feel many centers use “minimal access” as a marketing tool.
Adam: What type of procedures have you performed through an upper ministernotomy? Is it possible to perform a Ross Procedure via minimally invasive approach?
Dr. Jai Raman: Through an upper mini-sternotomy, I have performed:
- Complex aortic root reconstructions – using a valved conduit (both mechanical and tissue valves)
- Valve sparing aortic root reconstructions (modified David procedure)
- Redo aortic valve replacements
- Redo aortic root reconstructions
- Redo pulmonary valve replacements
At the present time, I have not performed a Ross procedure through that approach yet. But considering what we can do, I am confident that a Ross procedure can be done through an upper mini-sternotomy. Recently, I re-operated on a patient who had undergone a Ross procedure about 6 years ago and had a profoundly narrowed & scarred pulmonary valve. I reconstructed his pulmonary valve, right ventricular outflow tract and main pulmonary artery all the way up to the branches through an Arrowhead Mini-sternotomy.
Adam: I imagine there are times when a minimally invasive approach is not appropriate for a patient’s heart valve treatment. Why and when might that occur?
Dr. Jai Raman: There are few important contra-indications including:
- If the patient is unstable and we need open the chest quickly.
- If we need to perform bypass surgery along with valve surgery – though we have performed single bypasses on the right coronary artery through a minimally invasive approach
- Occasionally, if the anatomy of the patient is not suitable.
Adam: In those situations do you use a traditional sternotomy?
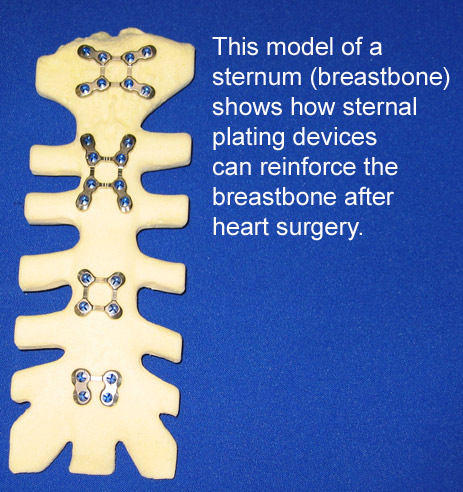
Dr. Jai Raman: Yes we do. Our sternal incisions have healed with very few complications because of the use of plate fixation.
Adam: Plate fixation? I have heard that the University of Chicago has pioneered the use of plates for accelerated sternal recovery. Can you explain more about that?
Dr. Jai Raman: When cardiac surgery came of age as a specialty in the 1950s, fractures of bones were being closed by lashing bony fragments together with wire. Wire closure of the sternum was adopted as a convenient technique and has persisted. However, over the past 20 years, all bone-handling surgeons have shifted to rigid fixation with plates. We have incorporated those techniques, worked with industry to modify plates for the sternum, on advice from our plastic surgeons. We have since developed experience with over 1,400 patients that have the plate fixation of their sternum and over 250 patients who have had ribs fixed with plates (for mini-thoracotomies). This use of plates has made closure in mini-sternotomies very easy and secure. The great thing about plate fixation of bones is that the break in the bone heals very securely with less pain and reduced risk of complications.
Adam: Looking into the future, do you see minimally invasive valve surgery changing? If so, how? Are there any particular technologies that you find encouraging or transformational?
Dr. Jai Raman: I see a bright future for minimally invasive surgery, where we incorporate techniques used in other surgical specialties and modify them for the heart. Already, I see the risk of surgery diminishing in terms of morbidity in the high-risk patients with minimally invasive approaches. Plating has transformed my practice. Also, the use of scopes – thoracoscopes for instance to aid visualization – have been very beneficial. A whole array of long-shafted instruments have helped. Better cannulae for peripheral cannulation and bypass have simplified the use of the heart lung machine.
Adam: Great! Thanks so much for chatting with me today. I really appreciate it!
Dr. Jai Raman: Thanks Adam. Keep up the excellent work!
|
Ludmila Khalid says on June 26th, 2010 at 1:53 pm |
|
Hi Adam, Best regards,Mila. |
 |
|
Tim says on June 26th, 2010 at 6:24 pm |
|
Adam and all, As a recent aortic valve replacement patient of Dr Donald Glower at Duke Univeristy, I know how great the MICS is for the patient and the family. I could not imagine the pain I would have felt if I had a sternotomy. My surgery was 5 weeks ago and I have been driving for about 3 weeks and my recovery has gone very well–except for very minor issues. For anyone looking at any type of cardiac surgery, I highly recommend checking out MICS. Not every doctor or medical center does it because of the limited amount of access to the heart so you do have to do your homework. Even among surgical practices you may only find only one doctor out of the entire group to perform a MICS. |
 |
|
Merilee Brown says on June 27th, 2010 at 12:27 am |
|
I have moderately severe aortic stenosis. My cardiologist says that I may need a valve replacement within probably about 18 months. I go yearly to see how I am progressing. He also indicated that if I can wait long enough that they may be able to do this procedure similarly to the stent surgeries, through a vein. This blog has been tremendously helpful in educating me a lot about what I am looking forward to. |
 |
|
Scott Barton says on June 27th, 2010 at 8:26 am |
|
I am told that the MICS procedure may only be utilized once. Is this true? |
 |
|
Cindy says on June 27th, 2010 at 9:34 pm |
|
I live in CA & went to NY for my valve surgery. My surgeon in NY was “in network” for my insurance. I had absolutely no problems with insurance coverage “cross country” and the paid for all of my cardiac rehab locally from late Feb through August!! I did send all my heart tests information to NY to be evaluated. If you know you are going to need a surgery… now would be a good time to start checking with your insurance policy & getting 2nd & 3rd … however many you want opinions for your particular heart valve situation. When I found my surgeon he wanted me to wait no longer than 6 mos. to avoid any further heart damage. My cardiologist here had a “wait as long as possible” plan in order to keep me off coumadin blood thinners. That was because the doctors here ALL recommended replacing the valve. I was able to have a REPAIR which means NO blood thinners. Had I done the “wait & see” method my heart would have had too much damage to allow a repair. It was a very difficult repair as it was .. I was very fortunate that my surgeon (Dr. David Adams) spent an EXTRA 4 hours on me!!! 8.5 hr surgery! They had expected it to be 4 hrs. |
 |
|
mort Krakow says on June 28th, 2010 at 1:04 pm |
|
Can the Maze procedure for atrial fibrillation be acomplished at the same time as a MICS for aortic valve replacement ? |
 |
|
Mary says on June 29th, 2010 at 3:16 pm |
|
My husband had undergone mitral valve surgery 6 months ago. We are having a problem with his left lung filling up with liquid. He has had to have it drained 3 times. Is this a common result from the surgery? and if so why does this happen? |
 |
|
Ryan says on July 7th, 2010 at 9:52 pm |
|
I am a cardiac anesthesiologist and I have to say, the MICS stuff sounds real sexy but if I am going to have valve surgery, please split my sternum ALL the way so the surgeon can have access to my heart and not try to do it through a keyhole. I know of at least 2 patients, young and healthy having CABG surgery died because of a mishap with the robot. For every patient that is driving 2 weeks after surgery there are 2 that are sick and short of breath. Until this surgery is so common that every surgeon in this country is doing it, I will remain skeptical of the few “experts” at Academic centers who take 12 hours to do a 3 hour operation and call it “Minimally Invasive”. Thanks but no thanks!!!! |
 |