“Aortic Stenosis… The Neglected Child” By Dr. Giovanni Ciuffo
By Adam Pick on January 31, 2010
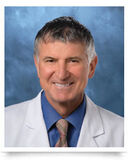
I recently met Dr. Giovanni Ciuffo, a cardiac surgeon at Mount Sinai Hospital in New York City. Although it was our first time chatting, I really enjoyed learning about Dr. Ciuffo’s practice which specializes in minimally-invasive heart valve surgery and, at times, bloodless surgery.
During our conversation, Dr. Ciuffo mentioned an article he just published about aortic valve stenosis and its impact on elderly patients. I found the article, “Aortic Stenosis – The Neglected Child: Novel Techniques To Take Care Of It”, full of educational and interesting information. That said, I thought you might like to review it as well. So, here are select excerpts from Dr. Ciuffo’s latest publication:
Calcific aortic valve stenosis (AS) is quite frequent in our population. A clear increase in prevalence is seen with age: 1-3% in patients aged 65-75 years, 2-4% in those aged 75-85 years, 4% in patients older than 85 years.
It is, without a question, a disease of the elderly with the exception of patients with bicuspid aortic valves who present with severe AS or Aortic Insufficiency (leaky valve) two decades earlier and the rare case of rheumatic valve disease.

Picture Of Calcified Bicuspid Aortic Valve
Most patients are diagnosed because of their symptoms of CHF (shortness of breath and fatigue), angina (chest pain) and syncope (fainting) or because of an obvious and loud systolic murmur heard on the chest with the stethoscope. The current guidelines of the American College of Cardiology are very clear about treatment options on these patients. Severe symptomatic aortic stenosis means that the aortic valve is so calcified and clogged up that it barely opens to allow blood flow from the heart to the rest of the body. It is a uniformly lethal condition.
Unless an effective mechanical relief is offered in the form of aortic valve replacement. There is NO medical treatment for this disease. Without surgery three quarters of these patients will die within three years of symptom onset. The first graph shows very eloquently the striking difference in survival between medical and surgical treatment.
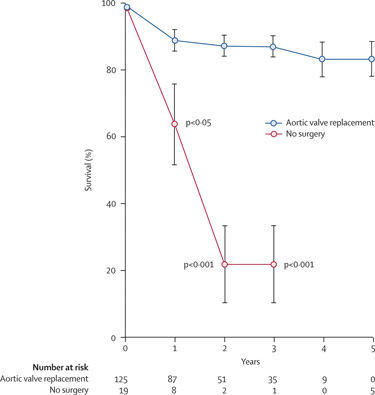
Survivability Rates: Medical versus Surgical (Aortic Valve Replacement)
Further, there is some urgency about taking care of it once symptoms ensue, since several reports have been published of sudden death within three months of onset of symptoms. In spite of these very well-established statistical data, severe aortic valve stenosis continues to be a grossly “neglected child” in our medical community. A good example is the all-too-common case of the little old lady who complains of worsening shortness of breath and ankle swelling.
Her doctor prescribes some Lasix (a diuretic) and she gets better. Two months later she shows up in the emergency room with recurrent CHF that resolves with intravenous Lasix. An Echocardiogram is obtained at this time and it shows severe or moderate-to-severe AS (Aortic Valve Area of 1.1 cm2 or less). This elderly patient and her family are reassured that some more Lasix will do the trick and that, after all, we do not want to rock the boat with a “dangerous” open heart operation.
Few more months go by and the family will call the office to let us know that Grandma has passed away and…well… to thank us for the wonderful care we delivered. There is a widespread and WRONG perception that surgery would not be a good option in an elderly and otherwise functional patient.
If we go back to the mortality rates I discussed, medical therapy is, by far, the most dangerous choice. The life expectancy of AS patients after an aortic valve replacement is the same as any cohort of patients without the diagnosis of AS. At one of my seminars, a local internist asked me if I would change my therapeutic indications in an old lady with several comorbidities (diabetes, hypertension, history of TIA’s). My answer was: “Let’s suppose this hypothetical lady with her comorbidities has mildly symptomatic colon CA (constipation) instead of severe AS….Would you be willing to send her home with a few fleet enemas instead of a referral to a general surgeon to undergo a “dangerous” colon resection? I don’t think so!!!”
Symptomatic severe AS, I might add, does kill you much faster than early colon CA. Let’s now consider our surgical options. A well-meaning relative will ask: “Isn’t Grandma too old and frail to withstand open heart surgery?” My answer is: “No. Grandma is too old and frail to withstand severe aortic valve stenosis. Let me show the statistics on this condition!!!”
The way I perform an aortic valve replacement in my service has dramatically changed the impact of this operation on the overall patient’s experience and on the speed of recovery. Most patients will be able to leave the hospital by their third postoperative day. A few pictures will illustrate this technique better than a thousand words. The surgical incision is about 2” in length and is carried out through the third intercostal space (in-between two ribs).

Minimally Invasive Aortic Valve Replacement Incision
There is no bone cutting involved and this is a great advantage for wound healing in patients with advanced osteoporosis. Furthermore, infection of these mini-thoracotomies is exceedingly rare. The entire operation and all the necessary connections to the heart-lung machine are carried out
through this tiny incision.
As you can see in the picture below, the prosthetic valve is ready to be tied in to replace the calcified valve and it is right at the center of my operative field. I routinely use the same incision for Atrial Septal Defect repairs, Mitral and Tricuspid Valve repairs, excision of atrial myxomas and tumors, Ventricular Septal Defect repairs, septal myectomies in IHSS patients.
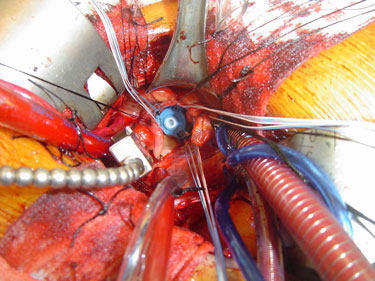
Prosthetic Aortic Valve Replacement Device
In female patients many of these operations can be performed through an incision hidden in the skin fold underneath the right breast with excellent cosmetic results.
Our patient recovers in the ICU and is extubated within the next 4-6 hours. On post-operative day #1 the drains are removed and most patients are transferred out of the ICU and start ambulation and physical therapy.
I hope these ideas will help colleagues, patients and concerned families achieve a real contemporary perception of what can be done for aortic stenosis patients of all ages. This low-impact, patient-centered approach to aortic stenosis affords excellent outcomes and restores a normal life expectancy and improved quality of life in the vast majority of treated patients.
If you would like to contact Dr. Giovanni Ciuffo, you can email him directly at giovanni.ciuffo@mountsinai.org or call his office directly at (212) 659-6800. Also, you can visit Dr. Ciuffo’s surgeon profile at our new Heart Valve Surgeon Database.
Thanks to Dr. Ciuffo for sharing his research with us!!
Keep on tickin!
Adam
|
Midge says on January 31st, 2010 at 8:32 pm |
|
This is a very informative article and should be available to anyone with aortic stenosis. I was fortunate to have a cardio who said very bluntly, “either have this surgery or you are going to die in the next few years, after having lived a very uncomfortable life up til then”. Was not too hard to make up my mind. This article really points up how successful this surgery is and how unsuccessful any other type of treatment can be. The surgery is not a picnic but it’s a wonderful alternative to doing nothing. Midge |
 |
|
Lucy Grubbs says on February 2nd, 2010 at 7:04 pm |
|
wow, this is soo informative, i do wish the medical profession would heed these warnings. I had warning signs and was misdiagnosed from a bicuspid valve, they all knew i had a heart murmur and would comment on it but never did anything, so I thought it was okay. Until i accidentally showed up at hospital w/a migraine and they found it did anything get done, and still, i switched cardiologists because one had a different view, because of my age, I’m 45, what should be done compared to the other. I am soo glad i switched, i ended up w/a ministernotomy 3 weeks after switching cardios, I went from considering surgery in the future with one cardiologist (not required right away) and my second opinion-what are you waiting for, you should have this done asap. I am glad i took the second route as when I was opened up, they said I would have had bad symptoms within 2 months! And that alone could have caused problems. I so wish other docs would read this article! |
 |
|
Dr. Ciuffo says on February 3rd, 2010 at 7:20 pm |
|
Thank you so much for your feedback on my writing. Your stories are great examples of what I discussed in my article. Midge: everybody is afraid of surgery and it is our job as surgeons and physicians to offer our patients WHAT THEY NEED and MAKE THEM UNDERSTAND WHY. Your cardiologist said it as it is!! |
 |
|
Chuck Bishop says on February 3rd, 2010 at 9:56 pm |
|
Dr. Ciuffo – |
 |
|
neil hitz says on February 3rd, 2010 at 9:59 pm |
|
Although absolutely no symptoms, had surgery for AS on Jan4. Valve was closed to 0.8. The plan was for Min Invasive ( as shown above), but my Dr wasn’t able to get valve to seat as he wanted, so did a full sternotomy and was also able to place a larger valve (St Jude #23 Epic Supra-Annular tissue valve). The point is that prior to sugery, I had differing medical opinions as to the pain levels for the 2 types of surgery. One week after surgery I went home & never took another pain med. Conclusion, ( for me anyway) with the right surgeon either procedure can be pain free. |
 |
|
Dr. Ciuffo says on February 5th, 2010 at 5:44 pm |
|
Chuck: In a patient your age, a biological valve tends to last much longer than in a 30 or 40 year old. Most heart valve surgeons would probably lean towards this choice for you rather than a mechanical valve and coumadin therapy. A reoperation 10-15 years later (if at all necessary) to replace a biological valve in an otherwise healthy 75-80 year-old man carries only a small increase in risk compared to the first operation. A minimally invasive approach through a mini thoracotomy the first time around can actually decrease the surgical risk in the future by offering the surgeon more options to expose the heart through relatively scar-free areas during the redo operation(i.e.: redo thoracotomy, median sternotomy, ministernotomy). In essence, you could have either type of valve replaced through a minithoracotomy and you do not need to be concerned about any additional redo risks related to this approach. Neil: I am not sure I understand why your valve could not be seated through a minimally invasive approach but you certainly had a good surgeon and a great outcome. As far as pain is concerned, the advantage of a minithoracotomy is that you can easily numb up that portion of the chest wall with local anesthesia and wake up right after surgery virtually pain-free. It would then feel mildly sore for a few days when the local anesthesia wears out |
 |
|
donna coogan says on February 9th, 2010 at 4:12 am |
|
i am a 52 year old woman from ireland who will be having aortic valve replacement in a couple of months..I WISH i could have it dont the non invasive way..amazing..great work ..heres to the future ways |
 |
|
Dr. Ciuffo says on February 9th, 2010 at 9:51 pm |
|
Donna, Here is a link about minimally invasive aortic valve surgery in Ireland: I hope that can help |
 |
|
cleat says on March 3rd, 2010 at 5:03 pm |
|
dr. ciuffo, i am a 53 yr old male who will be undergoing aortic valve replacement in may. i want to have the minimally invasive surgery that was mentioned in adams heart blog. how do i go about finding a surgeon in my area who can perform that surgery. thanks in advance for your help. |
 |
|
Dr. Ciuffo says on April 23rd, 2010 at 2:23 pm |
|
Dear Cleat, |
 |
|
diane says on November 10th, 2010 at 11:57 am |
|
My cardiologist neglected to tell me that she recommended a aortic valve replacement. I found out after I fainted@ a company picnic and was rushed to the hospital. Hard to believe she sent a ltr to my GP and recommened another test and valve replacement but didn’t tell me. To make matters worse I had to have back surgery 2 months after the diagnosis of severe aoetic stenosis and my GP signed off on a pre-op knowing I had this heart condition. Guess I was lucky twice. |
 |
|
Jack Castracani says on March 8th, 2011 at 9:29 am |
|
Dr. Ciuffo Would this prceedure work on someone that has already had a valve replacement? This is where I am right now. I have just left the hospital from pneumonia and while in the hospital I had an ultra sound on my heart which I had a valve replacement in late December of 2006. I learned in the hospital that my valve was closing and was placed on 24/7 3 liters of oxygen continuous. I just had my ultra sound from my cardiologist only 5 month previous to this and everything was fine and now to find that it is failing I was shocked to say the least. I also suffer from Lymphoma from having a 9.2 lb spleen taken out back in October of 2009. I have been on Prednizone (Steriod) since my spleen was taken out due to my body eating my red blood cells. I am just wondering if the Steriods had anything to do with my valve going bad and needing replacement. I am also alarmed at another operation for with my condition my platelets crash if I am off the Prednizone so I have to have the Steriods to produce them. My question is with my condition I would have to have all the medical treatment that I am getting now even after another valve replacement, but will they do another operation on me with my condition? I have to evaluate the situation with my doctors and find out what kind of time frame I have before this gets worse. I know if the last 5 months before I had this problem I was short of breath but I am on a pain management program with a 50 MCG Fentenyal patch and 4 mgs 6 times a day for break through pain of hydromorphone. The steriods have increased my weight by over 100 lbs not to mention that it makes my sugar levels go crazy so I take a nightly insulin shot to offset the steriod. I have now a pig valve but seeing this would be my 5th major operation and I am going to be 62 I cannot see myself doing this a third time if I get the chance to have another valve replacement. With all the medication I take I do not know if I would be able to use the coumadin with a mechanical valve. Any suggestions would be greatly appreciated for I am the deciding factor in this operation. I am so glad that I have found this forum for I know that I am not alone wth something that I knew nothing about. Good luck to all in this forum with any and all operations. |
 |
|
John Castracani says on March 11th, 2011 at 2:06 am |
|
After learning this past week after being in the hospital for phenomena and the doctors finding that my 4 year old aorta valve replacement is now narrowing fast from last November until now. I have so many doctors that are involved in this it is beginning to be a complication of one doctors opinion vs another. I have lymphoma and take steriods 40 mg per day to keep my body from eating my red blood cells. That said I also have other conditions as high blood pressure, CODP with risk of phenomena which I have had three times. I am getting frustrated for it seems that my hemotloigist wants to do a proceedure that is in IV form for 4 weeks and my pulmonary doctor wants me to wait until I am fully recovered from the phenomena , which I do agree, and then comes my gastrologist that is concerned with my hernia so I am in a wirlwind with doctors that are telling me nothing but fighting between themselves! I am concerned that my valve is in rapid deterioration and will need replacement but I am being kept in the dark with any and all proceedures while these doctors fight over me. I know I have to heal from being in the hospital for the breathing and cannot have an operation while being this weak. I also know that once I have this infusion IV with the hemotoligist is will take months for results if any to be seen. Now my cardiologist is just sitting back and letting everyone take over and saying that we have to do more test which I agree but in his words not mine this is a problem and we need do something but no rush?? I am just trying to get back on a road to recovery and without the valve replacement again this will not happen for they are just treating me with oxygen 24/7 3 liters continuous. I need a strong doctor which is not my GP to take charge and coordinate my health with these doctors and make decisions on my behalf and he is not doing this and to change a GP in midstream with my conditions will be suicide for me. What would you suggest on how to go about getting my condition under control and having this operation? I know what I want to do but that does not matter and I am at a point in my life that I am going to blow up at these doctors and tell all of them to go to hell but then where will I be? The fustration of being the patient and being on the outside of all these decisions is driving me crazy and I have four doctors perscribing medicine that they should not be and they have made mistakes on dosage with medicine like my steriod from my GP to take 80 mg a day which is way to much and I caught that! I need to get everyone in the same direction which is MY health and well being. Any suggestions on how I can go about this without blowing up at all the doctors at once? The final outcome that I want is to have this second operation of the heart valve replacement and be healing at home with some hope of leading a normal life for the next 10 to 12 years which will put me in my 70’s. Please let me know your feelings on how to go about this without everyone pushing me aside from any decisions. Thank you |
 |
|
Susan Byrd says on April 29th, 2012 at 10:19 pm |
|
Dr Ciuffo My 85 year old father was diagnosed twenty years AGO with a bad heart valve and was advised to have the “balloon” type proceedure done to repair it. My father is very stubborn and insisted he did not want it nor need it. I think he was very scared to have it done. He has been in pain the last year or so and says it has to do with his stomach. He sleeps a lot, has very little energy or strength. He mostly gets this pain after he eats. When we question him, he gets defensive, says he has been told by another doctor that his heart is “just fine” He went to a new “heart” doctor lat week and upon seeing his legs, told him blood was pooling in his legs!!!. He thought about this overnight and (finally)accepts it could be his heart after all, He has a follow up with this Doctor in a month!! My father is diabetic (oral medication) and tkes coumadin. If this was your patient, what would you advise???? needless to say this has us all terribly upset. I know he doesn’t want to upset my mother (who has early stage dementia). He needs to take care of this. soon!!!!! Thank you for any assistance you can give. Sincerely….. |
 |