“How Quickly Can Mitral Regurgitation Progress?” Asks Julie
Written By: Adam Pick, Patient Advocate, Author & Website Founder
Medical Expert: Craig Smith, MD, Chief of Cardiac Surgery, NewYork-Presbyterian / Columbia University Medical Center
Page Last Updated: June 6, 2025
I just received a great question from Julie about the progression of mitral regurgitation.
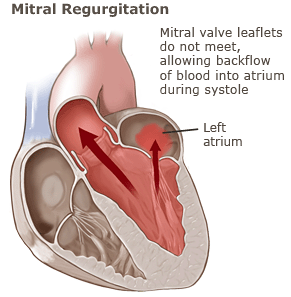
Julie writes, “Hi Adam – At 52, I was recently diagnosed with moderate regurgitation in my mitral valve. Even though I don’t have symptoms, I was diagnosed with a prolapse that I never even knew about until last week. Do you know how quickly the regurg can progress from moderate to severe? Is it a year? 5 years? 10 years? Thanks, Julie”
To provide Julie an expert opinion about mitral regurgitation progression, I reached out to Dr. Craig Smith, the Chairman of Surgery at NewYork-Presbyterian Hospital / Columbia University Medical Center. During his career, Dr. Smith has performed over 3,500 cardiac procedures — including more than 2,000 heart valve repair and heart valve replacement operation.
If you didn’t know… Dr. Smith’s former patients include Former President Bill Clinton (quadruple bypass) and Barbara Walters (aortic valve replacement).

Dr. Craig Smith
In response to Julie’s question about mitral regurgitation progression, Dr. Smith noted:
Moderate regurgitation with no symptoms may never require treatment. Mitral valve repair becomes important for severe, symptomatic regurgitation. Not all patients with severe regurgitation have symptoms, and valve repair is sometimes indicated in asymptomatic patients if tests show decreasing heart muscle function (left ventricular ejection fraction), worrisome enlargement of the pumping chamber (left ventricle), maladaptive response during a stress test, or atrial fibrillation. Once the regurgitation becomes severe, valve repair is more or less inevitable, although an asymptomatic patient who is carefully followed might have several years of safe waiting.
Dr. Smith then offered a helpful suggestion for Julie and other patients diagnosed with a leaking mitral valve.
It is very hard to generalize about the probability and time course of progression from moderate to severe, but the best protection is prudent observation with a cardiologist including echocardiograms at reasonable intervals (usually 6-12 months).
Thanks to Julie for her question and a special thanks to Dr. Craig Smith for sharing his clinical expertise with our patient and caregiver community.
Related Link:
Keep on tickin!
Adam
|
Nupur Andrews says on February 8th, 2012 at 1:47 pm |
|
Very interesting topic for those of us in the waiting room. I was diagnosed at 42 with moderate-severe regurgitation, it has been three years with no change so far. I was told I am looking at surgery within 10 years from diagnosis. In my case, it seems like surgery is pretty much inevitable, but we don’t know when. |
 |
|
Don Hull says on February 8th, 2012 at 5:58 pm |
|
My mitral regurgitation was first detected as a “murmur” by my family physician in May 2007. In January 2008, I was told by a cardiologist that I had a “Class 3” leakage (Class 4 is the worst)and that I would be facing surgery within five years. In January 2009, my cardiologist said it had worsened to a “Class 4” (severe) and that I needed surgery soon (within four months). My mitral valve was replaced in April, 2009. All the time, I never had any symptoms. Even the day before I reported for surgery, I worked six hours in the yard with no symptoms. I will admit though, that I was going through a lot of stress during the settlement of my father’s estate over an extended period of time, and even with medication, my blood pressure was borderline “high.” I’m glad I had the surgery. |
 |
|
Maria Williams says on February 8th, 2012 at 10:22 pm |
|
I was diagnosed with mild mitral valve prolapse when I was 33 yrs old. I did not need surgery until I was almost 64. I considered myself to be asymptomatic. At age 62 I was diagnosed with severe mitral valve regurgitation. After the surgery (repair) I now realize I did have moderate symptoms-slight fatigue, occasional shortness of breath but this was my normal. I am so glad that I had the surgery. It has been 14 months since surgery & my quality of life has significantly improved. I feel 10 years younger and I have so much more stamina. Continue your checkups with your cardiologist. |
 |
|
Travis Watson says on February 21st, 2012 at 2:45 pm |
|
I wondered the same thing before surgery and I still wonder 8 months after. I was completly asymptomatic and was never told of a murmur until I went to join the Navy at age 29. I swam in college and had physicals every year and was never told that I had a murmur. My murmur was a 5 on the 0-6 scale and my regurgitation (Mitral) was severe. This is why I wondered if this is something I’ve had my whole life or most of my life like the doctors said, or if this is something that occured much more recently. My cardiologist and surgeon said that the doctors giving me my physical in college and high school may have not paid much attention to my heart since I was an athlete in very good shape. All of this is speculation now 8 months after repair. One way that I though I’d be able to tell is after I’m COMPLETELY recovered from surgery, if I see a significant improvement in my run times and swim times, that could be an indication that my condition has been with me most of my life. On the other hand, if I don’t see much improvement it may tell me that the regurgitation was much much more recent, say in the past year or two even though doctors say this isn’t something that happens overnight. It’s now been 8 months post op, and although in the past 6 months I have made big progress, I am still not where I was prior to surgery. I do know that I am still not fully recovered so only time will tell. |
 |
|
Travis Watson says on February 21st, 2012 at 2:53 pm |
|
In addition to my above post, I wanted to say that it was one month from the time I found out about my reguritation until I was on the operating table. That was my choice though. I could have waited a year or so but it’s better to get it done before you do permanent damage to your heart. |
 |
|
Patricia Shabel says on March 4th, 2012 at 2:12 am |
|
I was born with mitral valve regurgitation, an enlarged heart, and a heart murmur. The doctors, then in 1965, wanted to put a catheter when I was a baby to see what was going on (exploratory), and my parents said no since it wasn’t going to correct the problem. I was very active as a child and as a young adult, so the doctors kept saying there was nothing to worry about unless it became a “problem” but no one said what that looked like. I tried to become a police officer when I was 24 yrs old but was turned down due to my heart murmur, even though I was in very good shape and health otherwise. The police dept cardiologist said I had moderate regurgitation and would need a “valve job” somewhere between 5 and 30 years from then, so they could not put me on the force, because the stress of the job would probably expedite the severity of the condition. I had mitral valve repair in December 2009 at 44 years old, almost exactly 20 years later when it finally became severe. Looking back, I was symptomatic from childhood with ADD-like behavior and inability to focus, which my surgeon, Dr. Trento at Cedars Sinai, said was a result of not getting enough blood and oxygen to my brain and would dramatically change immediately after the surgery, which it did. In July 2009, I went to my chiropractor and felt a “twang” in my chest and thought, that can’t be good. It turned out that the last of my chordea that was attached to my valve broke leaving me with a non-existent valve and no 2nd part to my heartbeat. That night, I ended up in the ER from almost passing out from dizziness and not being able to breathe. The dizziness had been going on for a long time, but I didn’t know it was related to my heart condition. The night before my surgery (5 months later), a friend told me later that my breathing sounded like that of a 90 year old woman. I was given the gifts of a normal beating heart & an ability to focus, for the 1st time in my life, and the symptoms are all gone and I am doing well today. |
 |
|
Sarah says on June 16th, 2012 at 4:40 am |
|
I have recently had an echocardiograph and my results came back as showing a mild mitral regurgitation. I’m not sure what the cause of this was, although I did suffer from scarlet fever as a 6 year old. I am now 31. My fear is that it will progress without me knowing. How long should be left between echoes and how long will it be before I need surgery to repair my mitral valve? Im feeling really scared. I have three small children (6 and under) and I hate the thought of not seeing them grow up! Could child birth have caused this damage? Any thoughts or opinions would be greatly appreciated. I also have an under active thyroid and take levothyroxine daily. I’m a little concerned that this might have an effect on my mitral valve. |
 |
|
victoria bocik says on August 29th, 2012 at 4:01 pm |
|
In 2010 I had unexpected open heart surgery to repair my mitral valve. I now have a mild leak in the mitral valve but feel fatigue, mild shortness of breath. rapid/skipped heart beats, a mild cough, and light headedness. Is this anything to be concerned about? I had a heart cath 2 days ago and my arteries look fine. Why am I experiencing these symptoms? Thank you for any thoughts on this. Victoria |
 |