Aortic Stenosis Progression: Top 5 Facts Patients Should Know
By Adam Pick on October 24, 2017
Aortic stenosis is a wildly misunderstood form of heart disease that impacts 12% of the elderly population. The disease is often mis-diagnosed and often under-treated. This narrowing of the aortic valve is commonly referred to as an “insidious” disease considering (i) its symptoms are regularly and incorrectly discounted to normal aging processes and (ii) patients can be asymptomatic. As the disease can have fatal implications, I’ve also heard several doctors call aortic stenosis a “silent killer”.

As my personal mission is to educate and empower our patient community, I wanted to learn more about aortic stenosis progression. Specifically, I wanted to dig deeper because so many aortic stenosis patients in our community are in “watchful waiting”. In watchful waiting, the patient has been diagnosed with aortic stenosis. However, the severity of the disease does not yet require surgical aortic valve replacement (SAVR) or transcatheter aortic valve replacement (TAVR). So you know… I was in the “watchful waiting” for 7 years.

To get patient-centric insights about aortic stenosis progression, I reached out to Dr. Kevin Accola, who is a cardiac surgeon at the AdventHealth Cardiovascular Institute (formerly Florida Hospital) in Orlando, Florida. Doctor Accola specializes in aortic valve surgery and has successfully treated many members in our community including Denise Ring, Geoff Gaskin, Scott Neiman, Duane Hunt, Barbara Coveny and Jeffrey Moore.
During our exchange, I asked Dr. Accola, “What are the top 5 things patients should know about aortic stenosis progression?” Here is his response — which includes an extra tip for the patients in our community.
Question #1: I was told I have mild-to-moderate aortic stenosis. How rapid may this progress?
Stenosis is the abnormal narrowing of a body channel, and in the case of aortic stenosis, it’s the narrowing of the aorta – the valve in the large blood vessel branching off the heart.
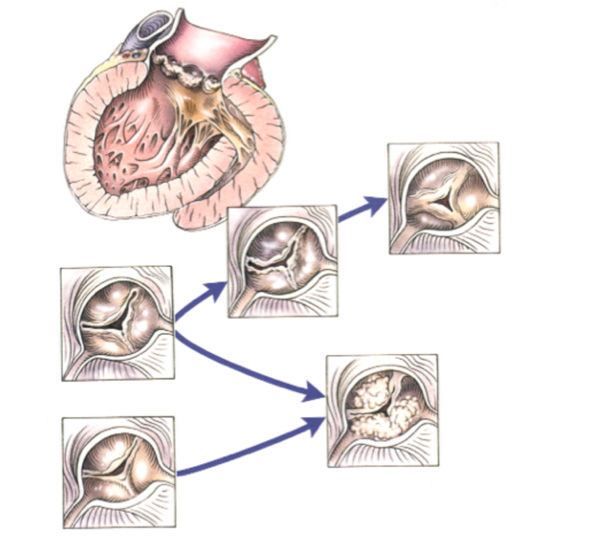
Degenerative aortic valve stenosis is a progressive disorder. The rate of stenosis, and the onset of symptoms may vary greatly in patients. (See the figure below demonstrating the progression of aortic sclerosis / stenosis.)
Question #2: Are there different types of aortic valvular disease or pathology?
Some patients may have a congenital variant, or bicuspid aortic stenosis, which can be hereditary. Often patients with a bicuspid aortic valvular disease present their condition and symptoms earlier in life, often with a mixture of stenosis and insufficiency.
Question #3: Can I do anything or take medicine to decrease the impact or progression of mild-to-moderate aortic stenosis, or prevent it from occurring?
As we age, this “degenerative sclerosis” of the aortic valve will continue to progress independent of what the patient does or does not do. Once the sclerotic process begins, there is no evidence to demonstrate any reduction or regression in this process and therefore must be followed annually with an echocardiogram evaluation to observe any interval changes in severity. The normal progression of aortic stenosis is from mild to moderate to… severe.
Question #4: What are the signs or symptoms when my aortic stenosis worsens, and what do I need to be aware of?
The significant symptoms of aortic stenosis are:
1) Shortness of breath.
2) Chest discomfort or anginal symptoms similar to coronary artery disease.
3) Dizziness or passing out.
Each of these symptoms clinically demonstrates a progression of the degenerative process and patients should see their physician promptly.
Question #5: I have been told my aortic stenosis has now gotten worse and will need my aortic valve replaced. What are some of my options?
There are various treatment options now available for severe aortic stenosis. In addition to conventional aortic valve replacement, select patients may be candidates for limited access or less invasive approaches. Transcatheter aortic valve replacement (TAVR) may also be an option in inoperable, high risk and intermediate risk patients.
There are also active clinical trials ongoing in low-risk individuals. These options can be discussed with your physician or cardiologist as well as your cardiovascular surgeon regarding which treatment strategy is available and most appropriate for each individualized patient.
I hope that helped you learn more about aortic stenosis, its progression, and your courses of action. I know it helped me! On behalf of our community, I wanted to thank Dr. Accola for sharing his clinical experience and research with our community.
- See Dr. Accola’s Interactive Surgeon Profile.
- Learn More About Aortic Stenosis Symptoms, Causes and Risks.
Keep on tickin!
Adam
|
Zack says on October 25th, 2017 at 12:17 am |
|
I appreciate Adam asking these questions of Dr. Accola. Now, I have one. I was diagnosed with aortic stenosis in 2016 and have been in the “watchful waiting” period for about 18 months. I am still trying to understand the criteria that doctors use in determining when the time has come to order valve replacement. Initially, I thought it was based solely on the valve area. When my valve area closed from 1.1cm (moderate) to .93cm (severe) in one year, I thought I’d be facing surgery soon. But the volume and velocity values were still on the border between mild and moderate, resulting in an overall “moderate stenosis” diagnosis by the cardiologist who read the echo. > My question: Do we wait until all three values are in the “severe” or a combination of “severe / very severe” categories before surgery is ordered? Over the past several months I have searched extensively for an answer to this question and have come up empty. There must be some kind of general formula that doctors use in determining when it’s time to act. I know it’s an individual analysis, but there’s got to be a generalized combination of factors that doctors use. Overall, I still feel pretty good. I wear a heart rate monitor to make sure I don’t overdo myself and I don’t get out of breath easily. I am 72 years old, reasonably active, and feel much younger. Thank you for the opportunity to comment and ask questions. More information reduces the stress we face. And, Adam, thank you for your website and your book. Both have helped me and many others who face this challenge. — Mark Wilbur (“Zack” on Disqus) |
 |
|
bermanhz says on October 4th, 2018 at 2:53 pm |
|
I have severe aortic stenosis with no symptoms. I exercise quite regularly with intense exercise 3x a week. I can walk for hours with no discomfort. Literature from the Journal of Cardiology says that one should wait for symptoms to occur before considering valve replacement. Any thoughts ? |
 |