Doctor Q&A: 6 Important Questions About Mitral Valve Surgery
By Adam Pick on December 3, 2019
My inbox is filling up with great questions about mitral valve disease and treatment. Lisa is asking about minimally invasive surgery and pain. Barbara asked me about the use of drugs to treat mitral valve disease and heart failure. And… Charles wants to know about cardiac rehab after mitral valve surgery.
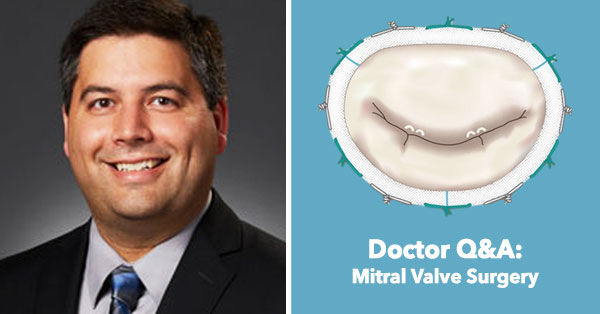
For these reasons, I reached out to Dr. Timothy George, a leading heart surgeon at The Heart Hospital Baylor Plano in Plano, Texas to learn more. So you know, Dr. George specializes in the mitral valve therapy and has successfully treated many patients in our community including Fred Riney, Anthony McDaniel and Diane Dean.
Why did you choose the mitral valve as a key specialty in your practice?
I consider it a great privilege to be a cardiac surgeon. I don’t think there is any other specialty in medicine where one can so dramatically improve a patient’s quantity and quality of life so profoundly with a single operation. This is particularly true of valve disease.
By the time patients with severe valve disease are referred for surgery, they are often literally incapacitated – they are unable to perform normal day-to-day activities, and their long-term survival is severely threatened. After valve surgery, our patients feel better and will most often return to a normal life expectancy. It is incredibly rewarding to achieve this with a single operation.
This significant impact is particularly evidence in mitral valve disease. Often patients with mitral valve dysfunction have had a gradual but profound decrease in their ability to enjoy life and many have had multiple hospitalizations for heart failure. With a single operation, we can get them back to doing what they want to do.
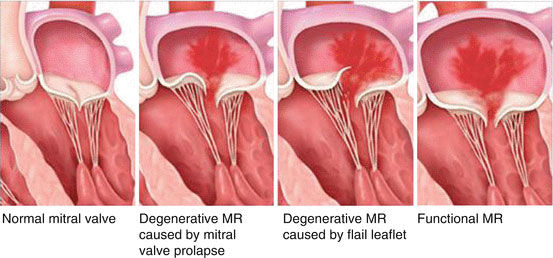
The other aspect of mitral valve disease that drew me specifically to this valve is the complexity involved in this valve. The mitral valve can be dysfunctional because the valve itself is damaged, what we call degenerative disease. In these cases, there are multiple different techniques that can be used to fix the valve. Sometimes the valve needs new cords, or the valve needs to be increased in size with a patch, or decreased in size with a resection, or resized with a band or a ring. Additionally, the valve can also be dysfunctional because the heart isn’t working correctly.
We call this functional mitral disease. Sometimes this is fixed with a valve repair, valve replacement, or Mitraclip but sometimes it can be fixed with medical management. This can make treating mitral valve disease challenging but also interesting.
Often, as a mitral valve surgeon, I can fix mitral disease without even operating by fixing other heart disease – blockages in coronary arteries, problems with the rhythm, better blood pressure control and heart failure management, etc. Mitral valve disease is both complex and challenging. Achieving a good, lasting result is extremely rewarding.
How have minimally invasive techniques impacted your approach to treating mitral valve disease?
I think in treating heart disease in general and mitral disease in particular, it’s important to use the right tool at the right time. The most important thing about mitral valve intervention is to get a good result safely. Therefore, my main goal is to do excellent surgery with zero mortality.
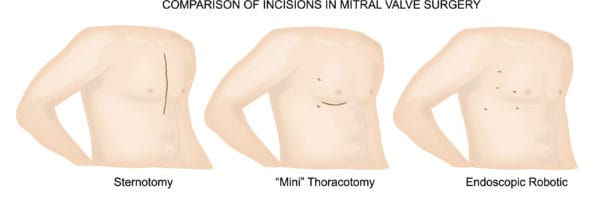
That said, here at The Heart Hospital in Plano, we are fortunate to have a very high volume of mitral valve disease. This has allowed our group to develop minimally invasive approaches to treating this complex disease process. In most cases, we can perform mitral valve repairs and replacements through a small incision on the side of the chest rather than through a traditional sternotomy in the front. This is true even in patients who have had prior, traditional heart surgery. In fact, our research has actually shown that in select patients, the minimally invasive approach is not just less invasive, it’s actually safer. So, our approach has been that we always perform safe surgery and in most cases that will be minimally invasive surgery.
What techniques does you team use to manage patient pain?
Unfortunately, pain can be a part of any surgery. Heart surgery is no exception. Fortunately, there are many ways to minimize post-operative pain. One important way to minimize pain is to do the surgery minimally invasively. At The Heart Hospital, most of our mitral valve surgery is performed minimally invasively through a small incision on the side of the chest rather than through the front of the chest.
The second part of our pain control regimen is a good nerve block. We are fortunate at our institution to have some of the best anesthesiologists I have ever worked with. They can perform a regional nerve block before the operation that significantly reduces post-operative pain. Not only does this reduce patient discomfort but it also reduces our patients need for traditional pain medicines including narcotics. This helps speed their recovery and decreases the risk of complications from narcotics including addiction.
Finally, we take a multi-modality approach to pain medicine. What that means is that we don’t just give patients narcotics; instead, we give them many different kinds of medicines with different mechanisms of dealing with pain.
Our experience has been that with a good, minimally invasive mitral surgery combined with a good nerve block and a multi-modality approach to post-operative pain management, most of our patients don’t need narcotics at the time of discharge. This translates into earlier discharges, faster return to work and leisure activity, and ultimately more time at home with family and friends.
How are transcatheter approaches to mitral valve therapy transforming your practice?
There are many new devices and therapies for treating mitral valve disease and there is no question that they are the future of mitral valve intervention. Currently, the transcatheter therapies are good and improving but not as good as mitral valve surgery. Therefore, I think it’s important to use these techniques appropriately. Most of these devices are approved for or being studied in patients who are too high risk for surgery. They are able to achieve an excellent outcome in patients who would have no other option. However, the current transcatheter techniques often leave some persistent mitral leak. New technologies are constantly becoming available and so this is a moving target.
At The Heart Hospital in Plano, we are fortunate to be involved in many of the clinical trials that are testing these devices. At our institution, the surgeons who perform mitral valve surgery are also very involved in the percutaneous or transcatheter mitral interventions. We are part of multidisciplinary team that runs a mitral valve clinic. This team is comprised of experts in mitral valve surgery, experts in interventional cardiology, and experts in echocardiography. Together, we try to make the best decision about the best therapy for each patient.
Throughout my career, I have been at three other major, academic institutions and I don’t think there’s anywhere else in the world where you could come to a clinic and have as many as 8 doctors – surgeons and cardiologists – evaluate your clinical situation and your valve disease and come up with a comprehensive plan for how to treat it. If the best option is a transcatheter option, the surgeons will strongly advocate for it. If the best option is surgery, the cardiologists will be the first to recommend it. We truly have a unique team that is focused on finding the best treatment for the individual patient.
I would say these transcatheter therapies are clearly the least invasive available, but they are not the best treatment for most people yet. However, we are committed to providing the best solution for each patient. As transcatheter therapies improve and the indications increase, we will continue to do more-and-more of these procedures. I think I can speak for all of my surgical colleagues when I say that our goal is to mitral valve specialists first and surgeons second. What I mean by that is that if the best therapy is something other than surgery, we support that and will advocate for it as part of the larger mitral team.
What is important for patients to know about heart failure and mitral valve disease?
Mitral valve disease is very complicated. There are essentially two different kinds of mitral valve disease. One type, which we call degenerative, is mitral disease in which there is a problem with the valve itself – a broken leaflet, broken cord, etc. This type of valve disease can cause symptoms of shortness of breath and fatigue which we collectively refer to as heart failure. In this scenario, a valve problem leads to heart failure. There is a second type of valve disease, which we call functional, in which the main problem is not a problem with the valve but with the pumping chamber of the heart. In these cases, heart failure is causing the mitral valve to leak.
These situations are the most complicated. Many of these patients will get better just by treating heart failure. I have seen many patients with a severely leaky mitral valve get started on appropriate heart failure medications and their mitral leak went away completely. That is why it is so important to have your mitral valve treated at a center with a lot of experience. There is a temptation to operate on these patients right away because their mitral valve is leaking severely. I am a cardiac surgeon. I love to do surgery. But if I can cure your mitral leak with a pill, I will.
After a patient is on the best medical therapy, if their mitral leak remains severe, that is when we consider fixing the mitral valve. There was a recent randomized controlled clinical trial called COAPT which demonstrated that in patients with heart failure and severe mitral regurgitation, the use of the Mitraclip was associated with better outcomes than medicine alone. This has really opened up an opportunity to treat a lot of sick patients with mitral valve intervention.

Finally, some of these patients have end stage heart failure that is refractory to medical management but their heart function is so poor that a mitral repair or replacement either performed transcatheter or by surgery is unlikely to help. For those patients, we can implant a permanent pump in their heart called a left ventricular assist device or LVAD. This is at the extreme end of the spectrum of treating mitral regurgitation but it is very effective at improving the quality of life and helping very sick patients live much longer lives.
Do you consider cardiac rehabilitation an important part of the patient journey?
Patients often ask about cardiac rehabilitation after surgery. Usually what they have in mind is physical rehab. Obviously, physical rehabilitation is an important part of the post-operative recovery process. However, cardiac rehab is at least as important. Cardiac rehab is a structured program designed to recondition the heart after a major operation. We recommend it for every patient for several reasons.

First, cardiac rehab helps a patient and his or her heart to be re-conditioned after heart surgery. Second, it often helps the patient build confidence. It’s natural for patients to be nervous and even tentative about engaging in physical activity after heart surgery. Because cardiac rehab occurs in a monitored and supervised setting, it can help patients gain confidence that physical activity is safe. Third, several studies have shown that cardiac rehab is associated with improved long-term survival. For all these reasons it is an integral part of our post-operative recovery plan and we recommend it for every patient.
I hope that helped you learn more about mitral valve disease, its treatment and the benefits of cardiac rehabilitation. Many thanks to Dr. Timothy George for sharing his clinical experiences and research specific to mitral valve disease treatment with our patient community.
Related articles:
- See Dr. George’s Interactive Surgeon Profile
- Phil Can Breathe Freely Thanks to the MitraClip
- Mitral Regurgitation: What Should Patients Know?
Keep on tickin!
Adam