Sternum Wires: Can I Get an MRI After Heart Surgery? What About Chest Wire Removal?
By Adam Pick on April 13, 2020
I just received two excellent questions about sternum wires and heart surgery from Kelly and Bob.
- Kelly asked me, “Can sternum wires cause issues with other medical procedures? I am attempting to get an MRI and the technician is concerned about the metal in my body.”
- Bob asked me, “It’s one year after surgery. I still have pain in my chest. It hurts constantly. I want to have the wires taken out. Is that possible? If so, what’s involved?”
To answer these questions, I contacted Dr. Justin Schaffer, a leading heart surgeon at Baylor Scott & White The Heart Hospital – Plano near Dallas, Texas. So you know, Dr. Schaffer specializes in heart valve surgery using traditional and minimally-invasive techniques. Dr. Schaffer has performed 3,000 cardiac procedures and has successfully treated many patients in our community including Jerry Sams, Pamela Hogue and Thomas Barton. Here are the highlights of my video interview with Dr. Schaffer:
Key Takeaways from Dr. Schaffer’s Interview
There are so many helpful points in Dr. Schaffer’s video, I wanted to jot them down quickly:
- Patients should have no issues getting an MRI after heart surgery that required the use of sternum wires.
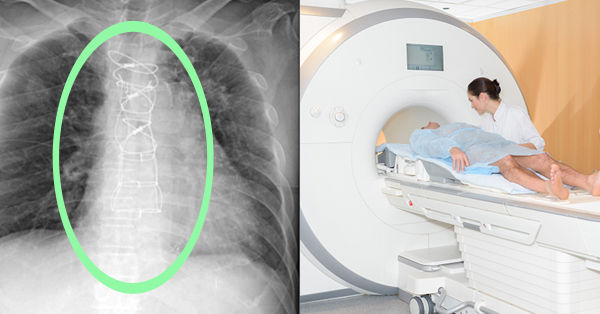
- Sternum wires are used during a sternotomy to help the breast bone heal. The wires are made from stainless steel or titanium. Metals exhibit different charges that are commonly referred to as ferromagnetic, paramagnetic or minimally-paramagnetic.
- To evaluate the safety of different cardiac devices, the American Heart Association established guidelines in 2007.
- MRISafety.com is a unique website where patients and health professionals can search for medical devices to determine their safety specific to MRI testing.
- Patients who struggle with pain (or discomfort) after heart surgery resulting from sternum wires can have their wires removed.
- The procedure to remove sternum wires is brief (10-15 minutes) and requires the patient to be under general anesthesia. The patient typically has some discomfort after the surgery. Most patients are in-and-out of the hospital during the same day.
- Dr. Schaffer typically performs 1-2 sternum wire removal procedures a year.
- Patients typically have favorable outcomes from sternum wire removal procedures. However, the outcome will not be known until the procedure is complete and the patient has healed.
Many thanks to Kelly and Bob for their questions. I hope this helped answer their questions about sternum wires. I also want to extend a special thanks to Dr. Justin Schaffer for sharing his research and his clinical experiences with our community! Thanks Dr. Schaffer!!!
Related posts:
- See Dr. Schaffer’s Interactive Surgeon Profile
- SternaLock Blu: Fast Healing & Less Pain After Heart Surgery
- What About Sternum Healing, Wires & Infection After Heart Surgery?
Keep on tickin!
Adam
P.S. For the hearing impaired members of our community, I have provided a written transcript below of my interview with Dr. Schaffer.
Adam Pick: Hi, everybody. It’s Adam with heartvalvesurgery.com. We are answering your questions in our Ask Adam Anything series. Today I’m thrilled to be joined by Dr. Justin Schaffer. Dr. Schaffer, are you there?
Dr. Schaffer: Thanks for having me, Adam – pleasure to be here.
Adam Pick: It’s great to have you. For folks out there, Dr. Schaffer, obviously, you’ve helped a lot of folks in our community, whether it’s Jerry Sams, Thomas Barton, or Pamela Hogue. I know you’ve done now, if I understand it, about 3,000 heart procedures. Is that correct?
Dr. Schaffer: That’s about right, give or take, Adam.
Adam Pick: Great, well, thanks for all the great work you’re doing. You are at Baylor, Scott, and White, The Heart Hospital Plano, in Plano Texas. It’s right next door to Dallas. Dr. Schaffer, we’ve got a lot of great questions coming in. Two are about sternal wires, those things that help keep your sternum together after you’ve had surgery. Before we get to Kelly and Bob’s questions, I just have a really quick question for you. Heart valve surgery is a very unique part of cardiac surgery. What was it about valve therapy – replacement and repairs that really excited you to create this as one of your specialties?
Dr. Schaffer: That’s a good question. Over the past 20 years, we’ve really seen a technological revolution in terms of the way that we treat valve disease, both from the terms of what we do from a surgical perspective, going from a more traditional sternotomy to more less invasive mini thoracotomies or robotic approaches, as well from more transcatheter approaches. It used to be that we could only fix coronary artery diseases with stents from an artery in the groin or the wrist. Now, we’ve developed technology to be able to fix a valve in the heart by getting there from an artery in the groin. That’s only improving. In the next 10 to 20 years, we’ll see a complete revolution in terms of the way we treat patients with valvular heart disease.
Adam Pick: No doubt it’s an exciting time. Dr. Schaffer, do you focus on one particular valve, or do you address all the valves in your practice?
Dr. Schaffer: Good question. I treat all valves, although I would say that about half of my practice is related to valves in the aortic position, or it’s related structures like the ascending aorta or aortic arch. This includes things like TAVRs or transcatheter aortic valve replacements, surgical valve replacements in people who don’t qualify for a TAVR because they need a mechanical valve, or their valve anatomy is not favorable for a TAVR. We do those through an upper mini-sternotomy, then things like aortic dissections or aortic aneurysms, valve sparing, aortic root replacements or even the Ross procedure. We do some mitral procedures from the more minimally invasive things. Then obviously, there’s also the regular bypass surgeries, like the traditional coronary artery bypass grafting and also robotic single-vessel approaches where we come in from the left side.
Adam Pick: We’ve got questions from Kelly and Bob all about sternum wires. Maybe you can real quickly help the patients out there understand what part of the procedure you use the sternum wires – exactly they’re used for and the success that you’ve had with them thus far.
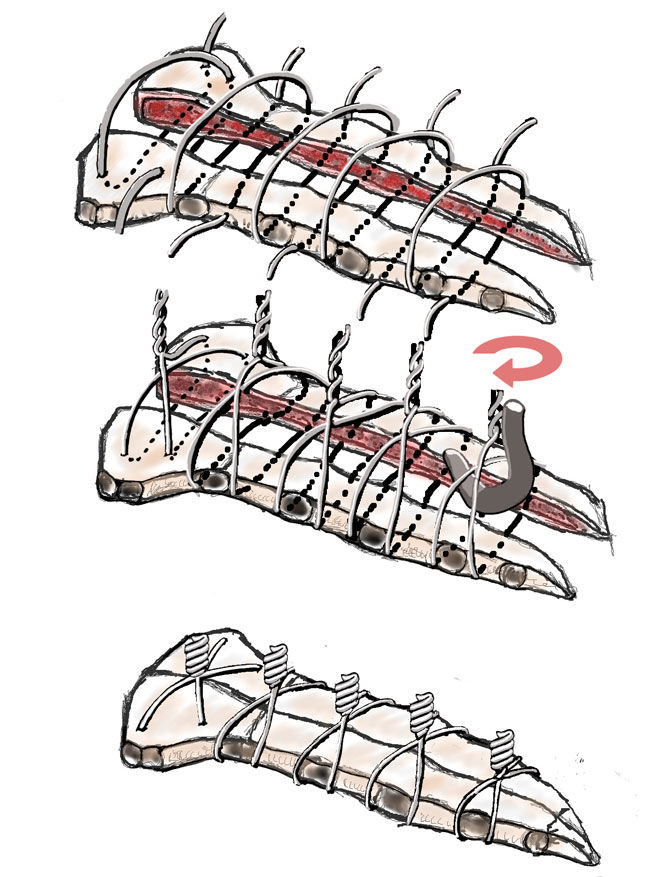
Dr. Schaffer: Sounds good. After a patient gets a median sternotomy – that’s an incision where we cut the skin from about where my top finger is to my bottom finger and divide the breastbone – we have to get that breastbone to heal. To get it to heal, you need both sides of the breastbone to be opposed, be together. That’s where either a sternal fixation system or a sternal wire comes into place. A sternal wire goes around the breastbone, from one side and the other, and allows us to twist the wire together and bring the sternum together. When that sternum is together, like any broken bone, it will mend to about 90 percent of its normal tensile strength about 8 to 10 weeks after the bone has been put together again.
At that point, the bone is essentially mended, and you don’t need the wires anymore. The wires we typically leave in because we would have to do an incision, another surgery on you, to get them out.
Adam Pick: Thanks for the overview. I’ve got sternum wires in me right now. We’ve got questions all about those sternum wires. The first one comes from Kelly. She asks, “Can sternum wires cause issues with other medical procedures? I am attempting to get an MRI, and the technician is concerned about the metal in my body.” What are your thoughts for Kelly?
Dr. Schaffer: That’s a great question, Kelly. I would say I encounter this question with either a clinic patient or someone in the hospital at least once every couple of weeks. The short and sweet answer to her question is, it is safe for Kelly to undergo an MRI procedure. Unfortunately, the devil’s a little bit in the details, and in medicine, we like to make everything as complex as we possibly can. I think it’s important for me to at least talk a little bit about the details, so it helps other folks with similar questions. In general, the wires that we put in to bring that breastbone together are either stainless steel or titanium based. That goes also for sternal fixation systems, which we sometimes use for patients.
Those metals are not ferromagnetic. Ferromagnetic means something that is highly charged and will have a strong attractive or repulsive force applied to it when it’s inside a magnetic field. Those are not what we see implanted in hearts at all. Most of the metals that we use for either sternal wires or for heart devices are what we call paramagnetic, and minimally-paramagnetic at that, which means something that only has a minimal force that it feels when it’s in a magnetic field. Because of that, most of these are essentially safe, but we hate to say safe for sure if something has not been rigorously tested.
That leads to the American Heart Association which has developed guidelines, which it did in 2007, to try and help us figure out what is an MRI safe device? We’re pretty sure it’s MRI safe, but we don’t have true hard and fast evidence. What is an MRI unsafe device? They paired with a website called www.MRIsafety.com. We’ll go over that a little bit later. You can actually look up whatever device is implanted in you. Basically an MRI-safe device would be something that has no magnetic items whatsoever. It’s nonmagnetic, a plastic something. That can’t feel any force in a magnetic field, so we know from basic physics, that it’s MRI safe.
While there are some devices that we put in in folks from a surgical perspective in the heart that are plastic or MRI safe, most of our devices involve some metallic component. Most of our devices are in this next category, MRI conditional. That’s an item that has never been demonstrated to pose a threat and that has been studied, but we can’t be 100 percent sure that it will be fine, but we think it’s going to be safe. It’s been tested in other MRI devices, and they haven’t had an issue with it. As long as you have an MRI technician doing your procedure who is following the guidelines for whatever MRI device they’re using, for all intents and purposes, should be safe, unless some bizarre, catastrophic event occurs.
That applies to almost any device that we implant in the heart, whether it’s a valve, or a stent, or these wires. Then lastly, there are MRI unsafe devices, which are the ferromagnetic devices, those devices that feel a very strong magnetic force when they’re inside a magnetic field that are MRI unsafe. Very few, if any, cardiac devices fall under that category. The good news is, there’s a website devoted to this. You can actually go to www.MRIsafety to actually look up your specific device to make sure that it’s okay.
Adam Pick: Dr. Schaffer, I can’t thank you enough for taking the time for the very detailed explanation because I get this question often. Finally, I’m going to have a video interview where I can share with our patient community that they can access this and feel better about the next steps in their therapeutic process. Thank you so much. Let’s shift now to Bob’s question. This is another question that I get asked all the time. Bob asked, “It’s one year after surgery. I still have pain in my chest. It hurts constantly. I want to have the wires taken out. Is that possible? If so, what’s involved?”
Dr. Schaffer: Another good question, Bob. I would say probably once a year or once every other year, I will remove somebody’s sternal wire. Yes, it can be done. It’s a very straightforward procedure. The big question is whether removing the wires will remove someone’s sternal pain. That’s something that, in general, we don’t know until we do it. I had one old surgeon when I was in training tell me that whenever you do surgery for someone who has pain, what you get is pain with a hole in it. Just be careful for doing surgery for pain. I have had a couple patients who had a really good outcome when removing the wires.
Adam Pick: What is the process for you to go ahead and remove the sternum wires for a patient?
Dr. Schaffer: Unfortunately, the only way to get the wires out is to do another incision. We have two options there. One is to make a small incision over each of the heads of the wires. The others is just to do an incision along the entire old incision. Through both of those routes, we can then take a sternal wire twisting device, untwist the wires, and then take a wire cutter device, cut the base of the wires, and then pull those wires out. Then what we will do is then suture that skin back together with absorbable suture, in general, something that would be absorbed by the body, so there would be no stitches on the outside.
It’s usually a 10 or 15-minute surgery. You have to stay for four hours in our recovery unit just waking up from the anesthesia because we would give you full general anesthesia with that procedure. Then folks can go home that same day. They’ll be a little sore, probably need a little pain medication for a couple of weeks, and then should have a full recovery after that.
Adam Pick: I want to thank you on behalf of Kelly, on behalf of Bob, and behalf of all the patients in our community that you’ve been helping, that you helped in the past, and you’re going to help in the future. We’re going to go ahead and put up your contact information. If anybody would like to schedule an appointment with Dr. Schaffer, you can call his office. I really hope everything continues to go great for you down in Plano, Dr. Schaffer. Thanks for being with us today.
Dr. Schaffer: Pleasure talking to you, Adam, and thanks for having me.