Ken’s Cardiac Catheterization Procedure – Insurance, Fear, Pain, Going Home
By Adam Pick on August 18, 2008
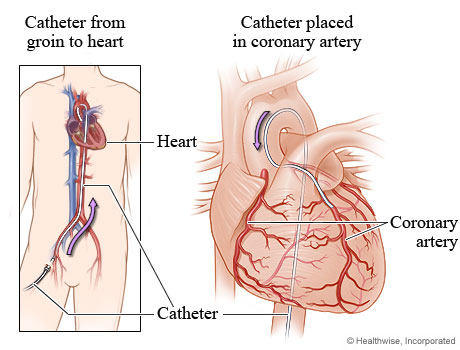
Considering that a cardiac catheterization is on Time Magazine’s “Top 10 Scary Medical Procedures”, I am always looking for good patient information to dispel the fear associated with this procedure. (FYI, many heart valve surgery patients have a cardiac catheterization prior to valve repair and valve replacement operations.)
On that note, Ken just sent me a very detailed account of his recent cardiac catheterization. So you know, Ken has severe mitral regurgitation and is scheduled for surgery later this month. As you can read below, he has some interesting points specific to insurance, fear, the procedure and going home afterwards.
Without further ado, here are Ken’s thoughts specific to his recent cardiac cathetherization:
Insurance Considerations For The Cardiac Catheterization
I am enrolled in an HMO and therefore needed referrals from my primary care physician for the cardiologist and the hospital. Since my cardiologist was performing the procedure at Massachusetts General Hospital, I also needed a referral for the admitting cardiologist there as well.
Massachusetts General will discharge day surgery patients as late as 10pm at night. If I had to stay overnight, I would have been liable for a $500 co-pay under my plan. Since my procedure was originally scheduled for mid- afternoon, I asked for an earlier time on another day. My cardiologist and the hospital were very understanding and accommodated my request. This required me to change the referral to a different admitting cardiologist.
Be prepared to coordinate everything among multiple, participating physicians. With the medical community’s ability to raise prices at will, it seems they have very little incentive to become more efficient.
My Fears & Concerns About The Catheter
I have small veins and people have trouble drawing my blood. During a blood test, two weeks earlier, it took two people, three tries to reach my vein. That left me with a bruise larger than a silver dollar.
Because doctors have not always told me the truth in the past, I did not know what to expect in terms of discomfort and pain from the catherization. Unable to find good information about catherizations on the web, I needlessly worked myself into a frenzy over the two punctures that would be made in my abdomen.
Given my experience with the “blood letters,” I was particularly worried about moving on the operating table and causing internal injury to my artery.
Being a “Type A” personality, I was even more so the day of the procedure. A double sedative failed to put me asleep. I’m sure the nursing staff was glad to see me finally go under. The medication caught up with me later that evening at home. After the procedure was over, I realized my fears were completely unjustified.
Procedure & Diagnosis
My cardiologist is exceptionally skilled and gentle. Everything went as planned. He had previously performed a TEE on me in September of 2007 with equal skill and will be performing another in 2 weeks.
This is how my procedure went:
I fasted after midnight but was allowed clear liquids up until 8am that morning. I had a small amount of water at 4am and again at 7am, and then nothing until after the procedure.
After check-in and completion of paperwork, I began getting ready around 11am.
I told the nurse who inserted the I.V. that it would be hard to find a good vein. She quickly terminated the first attempt and succeeded on the second try. Before being sedated, Dr. LaMattina came by and explained the risks of the procedure. He had me sign a consent form.
The procedure began around noon time. It took 35 minutes. Both an artery and a vein were explored right back to the heart. No blockages or calcification were found. No stents and no bypass surgery will be needed. I have a very strong and regular heartbeat. There is severe mitral regurgitation (over 60%) due to a prolapsed mitral valve which we knew about.
I was awake, apprehensive and talking (too much) throughout the procedure. I did not feel a thing, except when the warm dye was injected. I actually found that to be a rather pleasant feeling.
In the recovery area, a technician removed two plastic tubes (about 5-6 inches long) from my abdomen. It was painless. He applied pressure for about 10 – 15 minutes to each wound, then applied a clear bandage. Plugs were not used to seal the wounds because plugs could have delayed cardiac surgery.
My Transfer To A Regular Floor After The Cardiac Cath
The staff in recovery called ahead and warned the nurses what to expect. (Yak, Yak)
I had to keep my right leg still for at least 4 hours and could not bend it. My head could not more elevated more than 30 degrees. I forgot about this twice and moved the right leg slightly with no adverse effects.
I was given a delicious turkey sandwich lunch with lettuce, tomatoes, sweet pickles, grapes and apple juice. My wife had to help me because I could not elevate my head to feed myself properly. Drinking from the straw was the most awkward part of the meal.
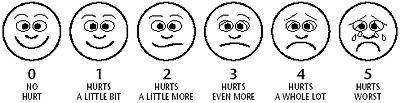
Before my release, a nurse took me for a walk around the floor. I initially had the very slightest amount of dizziness. The walk was pain free. I would say that the maximum amount of pain I felt that day was less than 1 on a pain scale of 1 to 10 with 10 being unbearable.
I was in a regular hospital room from about 1pm until discharge time at 6 PM.
I recommend that patients bring a book or watch TV to pass the time. My wife had a book. Being the type of person who must keep busy, I was still hyperactive. If I could have had my laptop with me, I would have been fine, but my recovery position made that impossible.
Despite the volume of people they service, the entire staff at Mass General is very professional and attentive. I would be remiss, however, if I did not single out Ms. Kim Powers, a physician’s assistant who extremely proficient and caring. Despite a caseload that changes daily, she does an excellent job of keeping up with everyone’s progress by personally visiting each patient under her care before and after their procedure. If you are fortunate enough to be assigned to her care, appreciate the fact that you are receiving a level of care that does not exist everywhere.
Finally… Going Home!
We carefully monitored the groin area for puffing and internal bleeding in the lower abdomen. To avoid climbing stairs, I slept on a couch the first two nights. My sleep has been choppy for some time because of the heart valve issue.
I went to bed at 8pm that first evening and fell asleep without any need for Tylenol or other pain medication. I woke up around 2am, as I usually do, but did not feel any discomfort at all throughout the night.
During the first 24 hours, a very small amount of blood leaked where the upper leg and abdomen meet. The clear bandage that was applied after surgery was lifted slightly at the crease. My jockey shorts acted like a wick and absorbed the blood.
The day after the procedure some linear bruising began to appear in this area.
The afternoon of day 2, my wife helped remove the bandage, as directed, and I was able to shower. To get upstairs to the shower, I took it one step at a time. Pushing down on a railing, I put my weight on the good leg and lifted it first. Then I brought the affected leg up to the same step. This was precautionary.
For the first two days after, I tried not to bend my right leg. I had trouble putting on my trousers and could not put on my socks either day. The morning of the second day, my pain level went from negligible to 1 out of 10. More bruising was evident but not anything significant. Over the next few days, it became larger and spread toward the hip area.
No swelling or internal bleeding was observed. By the afternoon of day 3, all pain was gone. I was also moving up and down stairs very fluidly. I took it easy, as advised in the discharge papers, for a full week. Some bruising remains after a week, but I now healing.
I am now looking forward to the heavy duty mitral valve surgery in three weeks and hope to be a better patient. I will be completely under anesthesia and am prepared to deal with the associated issues when I awake.
So far I have not experienced any form of depression after my cardiac catherterization.
I hope this helps future patients and caregivers!
Adam… Thanks again for your heart valve surgery book!
Ken
|
nancy mallinger says on August 18th, 2008 at 9:15 pm |
|
I had a cardiac cath 50 years ago, when I was only 8, and was severely traumatized because they used very little anesthesia and I was wide awake. In addition, the procedure was very different–needles were inserted directly into several areas in my chest, and I felt and heard everything. I know they do things totally differently today, but is it any wonder that I think I am dreading the cath almost as much as the surgery I will have in November? I appreciated reading about your experiences. Maybe it won’t be as bad as I am expecting. |
 |
|
Barbara Girga says on August 19th, 2008 at 2:53 pm |
|
I had my procedure Friday, and like you, was frightened by media reports, etc. Sticking something like a camera into my groin area didn’t seem like anything pleasant, but my 4 months of absolute fatigue, and other symptoms made it clear that I needed help to find out the problem. In the middle of the exam, my wonderful cardiologist smiled and said “good news. The heart is fine.” I was a tad disappointed(3 secons maybe) because now we had to do more research on my problem. Next will be the lungs, but I won’t get myself into a tailspin again. I trust my doctors, and all who are going to be by my side. This body dysfunction has left me with a wonderful lesson: I can’t always control everything, so let go and let the experts take over. I don’t try to be all things to all people, anymore. When I can’t breathe much, or tire after 3 steps, I take care of myself, and don’t worry what others think. All because of the trust I have now learned from having a Cardiac Cathererization Procedure. Barbara |
 |
|
Debbi Rose says on August 19th, 2008 at 5:11 pm |
|
Had my TEE last Thursday,sent me immediatly for PAT’s. Cath done the next morning, all out-patient. Virtually no discomfort, good results. aortic valve replacement ASAP in Norfolk Sentara. Don’t let anxiety add to your procedure. I didn’t have time to worry, and I’m glad to tell you worry is unnecessary. Get healthy and as Adam says, “keep tickin’!” |
 |
|
D B says on August 23rd, 2008 at 10:13 pm |
|
I agree that thought of what they’re doing to you is more unsettling than any pain associated with the procedure. The most uncomfortable part of the procedure was the slow regrowth of groin hair which is completely removed. Expect about a 3 month replenishment period. |
 |
|
lori says on January 1st, 2009 at 11:32 pm |
|
i just had the procedure done in mid dec.08, and it all went well, except when they were removing the catheter, there was a lot of pain. i ended up with a large bruised area from the groin area to the hip, due to a bleed-out, but they clamped me and stopped the bleed. however, three weeks later and i have this ‘bump’ the size of half of the baby finger on a person’s hand. its right in the groin area. no discomfort noted. i will be seeing my doctor soon to discuss the results and of course this ‘bump’. it feels cylindrical and im wondering if something was left behind?! i know i didnt need a stent, so what is it? hmmm soon to find out. |
 |
|
Wilmer David Brown says on January 4th, 2009 at 11:02 am |
|
I had a Cat in June 2005, I was asleep the whole time. I had another in May 2008, I was awake on that one. Both reveled no clogged artireies, no complications. June 2 2008 i had my Aortic Heart Valve replaced with a St. Judes Mechanical Valve. No stents were needed. i have a lot of ticking i can hear but I’ll start worrying when I can’t hear it. This was done at John Hopkins Hospital, Baltimore MD. I would suggest that if you have been told you need one, get it for it could save you a lot of pain and discomfort as time goes by. June 2 2008 was my Birthday, what better of a present than a new lease on life! |
 |
|
nancy mallinger says on January 4th, 2009 at 6:20 pm |
|
I had my cath in October. I had to wait for five hours at the hospital and was so scared that I cried almost the whole time. I begged them to give me something to calm me down during that time, but they wouldn’t. They did promise, though, that I would be basically out of it during the procedure. Unfortunately, they were wrong–maybe because I was so worked up, but after giving me meds twice (I think ativan and versad), I was still totally awake. The procedure itself was painless and no big deal, as was my recovery from it. Too bad that I didn’t know that going in. |
 |
|
Midge says on January 4th, 2009 at 8:12 pm |
|
Hi everyone. I’m a 67 yr old female who was diagnosed with Aortic Stenosis in Dec. 07. Cardiologist wanted to wait until it got worse before doing surgery. Saw him again in December 08 and he says it’s time to do a cath, which is scheduled for Jan. 9th. He is definitely of the opinion that the valve is now ready to be replaced but the cath will reveal any other problems so we can take care of them at the same time…hopefully there will be none. I just found Adam’s blog and ordered his book, but find the input from all of you of great benefit. At least I’m not anxious about the cath (maybe just a teeny), but as my doctor so aptly put it, you have the valve replacement or you die alot sooner than you should. Not hard to make a decision when you look at it that way. Just wanted to let you all know that your feedback is great for all of us “pending”. |
 |
|
Helen Hobart says on January 16th, 2009 at 10:05 pm |
|
I’m looking for info about risk factors of having an angiogram since I’ve had two minor strokes (2 yrs ago). My ekg shows a small dip that is questionable and my father, an overweight, stressed smoker, had a heart attack at 45 (lived to 86 without another). The relatively young cardio doc doesn’t want to take any risks and feels no other tests are as good as angiogram. I’m in good shape, 62, blood work a-ok, exercise almost daily, pretty relaxed, slim etc etc etc — any ideas or info for making this decision? |
 |
|
Randall says on January 21st, 2009 at 11:45 pm |
|
I had an angiogram done from my right wrist two days ago. I sorry to say it was the most painful experience of my life. It felt like my arm was being crushed in a vice. When the dye was injected it felt like my entire body was on fire from the inside. I have a high threshold of pain, but this was unreal. At some point I passed out. When I came around again the cath lab tech. was shaking me and yelling at me to get me to respond. I remember the cardiologist saying that I needed atropine and nitroglycerine. Nobody would tell me what happened. The results were negative which is good. I would like to know what happened to me. I’m a 46 year old man in good condition and I dont want to dothis again. |
 |
|
Marcia Jean says on February 7th, 2009 at 7:49 pm |
|
I am interested in experience of any post polio patient who has had a DYE angiogram. I am 65 and have occasional chest pains and upper left arm pain, occasionally pass out, bad circulation and difficulty with anestetics. In the last 2 years I’ve had both knees and lower back operations. No post op problems with knees, but different hospital for back surgery and had problems with post op recovery. They did keep me overnight but discharged me the following morning shortly after vomiting. We live on an island and it was a 3 hour wait, in the car, before a ferry and then 1 1/4 hr ferry ride. I became VERY cold, shaking, and light headed. I now have swelling in both lower legs and numb toes on each foot. (I think it was due to “pressure hose” being left on and sitting so long but surgeon pooh-poohed it,) I need to have tests done for heart disease but distrust the dye, etc. because of the post polio problems I have. I would appreciate any info or experiences from post polio people. |
 |
|
Connie Barlow says on May 12th, 2009 at 1:30 am |
|
My biggest concern is kidney damage… I know of one case in which the patient (my Mother’s 80ish husband) ended up on dialysis for the remainder of his life due to the dye damage to the kidneys. How frequently does this happen? I have my procedure scheduled in a week – am 66 – and following what was descr bed to me as a “significant” heart attack. Now fence-sitting as to the need for this invasive procedure, especially with its negative and adverse possibilities. |
 |
|
Midge says on May 12th, 2009 at 9:52 pm |
|
Connie, I’m 67 yr old female and had a cardiac cath in Jan. 09, followed by aortic valve replacement in February. I would guess the risk of problems with a cath are very minimal. Of course, I don’t know but there is inherent risk in every minute of our lives and when there is this marvelous equipment that can tell doctors so much so that they can perform surgeries to save us, I went for it without a second thought. My biggest fear of the cath is that I read the room is kept cold and I Hate Being Cold. When they got me in the procedure room, they brought these very toasty, fuzzy blankets and wrapped me up except for my head and the leg they were using. Only thing I felt was a small prick where they deaden the area where they are going in. Otherwise I was awake for the whole thing, did not feel anything snaking around my artery into my heart but got to watch a great show on the monitor of the inside of my heart. WHAT A TRIP! Spent a few hours in recovery with a clamp thingy on my leg which got changed to a “sandbag” toward the end. The gurney wasn’t super comfortable but it worked. Then they sent me home with a list of instructions that gave me an excuse to lie in bed and read for a couple of days. While I was still going thru the cath procedure, the doctor doing it was very up front with saying, “Yep, it’s time to change that valve.” Anywhere along the line, things can go wrong. But with the hundreds of thousands of these things done every year in the U.S. I bet percentages of problems are really small. Maybe Adam has a better idea of numbers. Good luck. Midge |
 |
|
LAurie Collins says on May 13th, 2009 at 2:42 pm |
|
Ken, |
 |
|
Mary says on August 25th, 2009 at 10:32 am |
|
Thank you for writing about your cath experience. I’ve had two, one in 86’and 96′. I watched both on the screen in Surgery. Was pretty cool to see what they did. (Guess I’m weird!, but wanted to see what was going on.) Back then I had to lay still for 8-12 hours! I am now 72 years old and still going strong with no heart problems. So those facing a cath, have no fear. God is in control and all will be good. |
 |
|
Ron Rogers says on August 15th, 2010 at 7:03 pm |
|
I just had an angiogram last Wed. the 11th of Aug. 2010. I am 66 and pretty much knew what to expect from experiences of others but was still scared as hell. I am a very modest person and didn’t much like the idea of laying there as naked as a newborn. Anyway, long story short, the procedure was very easy and painless. Dr. and nurses kept me covered whole time. I was wide awake the whole time. The hardest part was having to lay still for 5 hours afterwards. (Bad back). God Bless all of you. Hope your procedure was as easy as mine. Ron |
 |
|
Sherry says on March 28th, 2011 at 1:15 pm |
|
I have aortic stenosis due to a bicuspid valve that was not discovered until I was 55 years old. I was followed by a cardiologist for several years with regular echocardiograms which always showed mild stenosis. About three years into it, my cardiologist became very concerned about how my echo looked and we were planning a necessary trip of 2000 miles shortly. He insisted it was time to do a cardiac cath to determine how progressed the stenosis was. I worked in the medical field for 25 years, so little of it actually scares me, though it is certainly unnerving to know a wire is being threaded into your heart. The staff at the hospital explained everything to us so we knew what to expect. As others have said, it was fascinating to watch the screen as the test was performed; almost an out of body experience you will. Indeed, the hardest part is the prolonged rest afterward, but my husband helped me pass the time and I would doze off now and again. The after effects were minimal and I was given the clearance to leave on our extended trip four days later, with no problems. Things I learned: The catheterization showed that there had not been significant change in the stenosis since my diagnosis three years prior, which was a Hallaluliah moment! I had not been completely comfortable with my cardiologist for the years I had been seeing him, but since the answer at each visit was “stable, no changes” I stuck with him. He seemed unsure of things sometimes, and we had had a couple of times when the echo results didn’t seem right!? I took this scare as my nudge from above to find a cardiologist in whom I found a good raport and trust. I am now 60 years old, seeing a cardiologist that I have trust in, and there is no surgery in sight at this time. Be sure you are working with a doctor that you are comfortable with; it makes all the difference in going through the process of a progressive issue. I learned this through a diagnosis of cancer coinciding with the stenosis issue. |
 |
|
Doug says on April 4th, 2011 at 9:02 pm |
|
I have tow caths within the last 60 days. The first cath was in the groin which was just a bit more uncomfortable than the second which was through the wrist. I was given a mild seditaive on both occasions which was fine for me. It was not bad at all. Trust me when I say that because I am a BIG BABY and it really was ok. Thankfully, I have no significant blockage in my arterys (first cath done at Northside Hospital in Canton Georgia revealed 70% blockage in one artery, second cath done at St. Joseph Hospital in Atlanta, GA revealed slight blockage of 30% which is not enough to even address),however I do have to have my aortic valve replaced due to stenosis and mitral valve repair due to severe regurgitation. My advice to you all? Don’t sweat the cath, It was easy compared to what lies ahead for me! 😉 Doug |
 |
|
AT says on April 23rd, 2011 at 2:34 am |
|
People who are deathly scared of the procedure go to small town podunk hospitals to have this done…I would be scared too if I got it done at Barney Fife Memorial Hospital. Large teaching facilities are the way to go if you don’t want to be scared out of your mind. |
 |
|
roberta enyart says on August 8th, 2011 at 2:24 am |
|
i had a angiogram on dec. 1,1908, i went into the emergency room and they decided to keep me. i had shortness of breath, bp was 160 and swollen ankles. they decided to do an angiogram. while i was in the lab it caused a cariac arrest. code blue. 10 minutes before the doctor came out and told my family that i had 40% blockage. then they were told that i was in serios condition and they weren’t sure i would make it. i have a stent in the major value in my heart, i have conjective heart failure and a damaged heart muscle. i did not have any heart problems prior to this. i was told that they went through both groins to both sides on my heart, i don’t know if this is normal procedure. when the doctor went in to put th stent in i was cut and had to have 22 stitches. i’m also a diabetic. i wish i had asked more questions. i wish i had checked on other procedures before i had the angiogram. beware, asked lots of questions. and don’t let anyone tell you theirs little risk. i had been to my internist 2 days before and was never told that i had conjestive heart failure. yet this what i was told. i wonder if conjestive heart failure can come on that fast. |
 |
|
Jen LaMotte says on August 29th, 2011 at 8:55 pm |
|
I just want to say Thank you so much for your story on your catherization. I go for mine in 2 days and I was scared to death. You have helped me with my fears. Hope mine goes as well as yours did. 🙂 |
 |
|
Sandra Smith says on December 14th, 2011 at 8:02 pm |
|
I’m 65 yrs old and had an angiogram 3 days ago. I am in Australia so my experience may be a little different to in the U.S. I wasn’t worried about having the angiogram because I heard it was painless (and it was), but I had a small complication, which I don’t think has been mentioned in the other comments here. When a nurse attempted to get me up in the standard time after the procedure – 3 1/2 hrs, blood poured from the incision in my groin and there was general mayhem on the ward in an effort to stem the flow. It was all over the bed, the floor, my hands, etc. As you realise, the femoral artery is a major one and the cardiologist and 3 nurses all worked to get it under control. It scared me no end and I was so afraid to move a muscle for the rest of the day in case it happened again. I was kept in hospital for a further 24 hrs to monitor this. I am fine now, but the bruising across my groin is huge and black (probably from the pressure that had to be applied during the bleed). It’s just something to watch out for and keeping extremely still after the procedure is very important. |
 |
|
Jackie Black says on March 15th, 2012 at 12:24 am |
|
I am a 46 year old female and I had a regular stress test then a nuclear stress test. Both of these showed Ischemia. The cardiac doctor wants to do a cardiac cauterization. I am a bit worried but this site helped…a bit. I have been experiencing pressure in the area of my solar plexus and get tired going up stairs or walking. I push through it and it gets better. I am 5′ 10 ins, have high blood pressure and weigh 210lbs which puts me in the obese category. Any advice for the procedure versus trying some medication.BTW, my cholesterol is good, both hdl and ldl. |
 |
|
marcelle says on August 9th, 2012 at 2:46 pm |
|
I had my mitral valve replaced at 43 and had angiogram/cath about a week before my surgery. I thought it was really interesting to ‘feel’ my circulatory system (the warm flush of the dye) – definitely the highlight of that day which included a TEE. It was bittersweet though because the doctor who performed the procedure said “Your arteries are amazingly clean, I don’t see arteries this clean on people half your age.” “Too bad about those valves.” Still I guess its nice to know that my vascular system is in good shape :-). |
 |
|
Linda Sime says on August 9th, 2012 at 3:10 pm |
|
I had my TEE and Heart Cath all done in the same day. First the TEE, then the Cath 45 minutes after the TEE. No problem with either test. Groin a bit sore after after the Cath, but certainly walked out on my own within two hours after the last test and a great turkey sandwich! I did have a caregiver stay over night that night as added precaution. LS |
 |