Rapid Recovery Protocol 2.0: What Should Heart Surgery Patients Know?
Written By: Adam Pick, Patient Advocate & Author
Medical Expert: Dr. Marc Gerdisch, Chief of Cardiac Surgery at Franciscan Health
Published: June 26, 2023
Something fascinating is happening in cardiac surgery.
Thanks to new approaches in pre- and post-operative care, patient recovery processes are accelerating. In fact, a convergence in recovery benefits are transitioning from minimally-invasive to traditional open-heart procedures.
To learn more, we interviewed Dr. Marc Gerdisch, the Chief of Cardiac Surgery at Franciscan Health in Indianapolis, Indiana. During his extraordinary career, Dr. Gerdisch has performed over 6,000 cardiac procedures and successfully treated more than 100 patients in our community.
Key Learnings About Rapid Recovery 2.0
Here are key learnings from Dr. Gerdisch specific to Rapid Recovery Protocol 2.0:
- Dr. Gerdisch and his team developed a unique program to help restore patient quality-of-life after heart surgery. Dr. Gerdisch states, “We started a very aggressive program of patient recovery that expedited getting out of the hospital, getting back to your life, and being fully active.”
- Initially, the recovery program focused on patients who underwent minimally-invasive therapies. However, Dr. Gerdisch felt there was a significant opportunity to transfer the learnings from minimally-invasive surgery to open-heart procedures.
- A critical component of the Rapid Recovery Protocol 2.0 is the use of rigid sternal fixation. Dr. Gerdisch states, “The first thing we did, that foundational building block, was to move toward everyone having rigid plate fixation of the sternum. Everybody has an orthopedic repair of the bone, the divided bone, so that we take the bone out of the equation.”
 Rigid Sternal Fixation
Rigid Sternal Fixation
- When patients get rigid sternal fixation, their pain levels and their use of narcotics dramatically decrease. “We saw patient pain go way down, to the point where we reduced the use of opioids by 96 percent,” states Dr. Gerdisch.
- With less pain and less medication, Dr. Gerdisch can extubate patients while in the operating room. “More and more patients come out of the operating room, no matter what the approach is, already off the ventilator,” states Dr. Gerdisch. “They’re comfortable. They can be off the ventilator. They can breathe.”
- Patients get out of bed and start walking shortly after surgery under the Rapid Recovery Protocol 2.0. Doctor Gerdisch states, “Within four hours, the patient gets up out of bed. What it does is it lets them recognize they have not been disabled by the operation. Next day, up in the morning, nobody gets back in bed all day; they’re up walking. All that is achieved not only because we’ve done rigid sternal fixation and because we’ve decreased the need for those medications.”
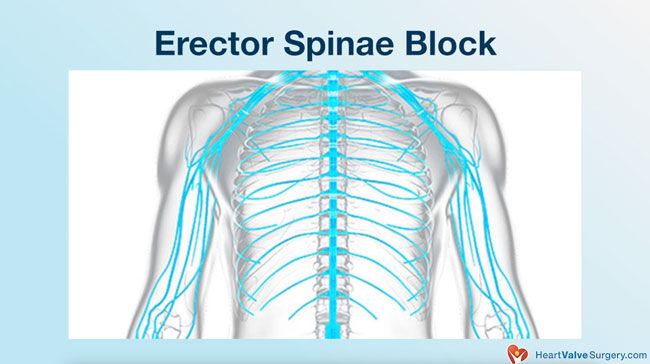
- To further minimize pain, patients receive an erector spinae block. As a result, patients can use their arms more freely, enabling patients to lift items and drive sooner. Doctor Gerdisch states, “Day after surgery, up to 15 pounds in each arm. Basically, over the next few weeks we let you get up to 25 pounds in each arm. The other thing that we recognized was that with that mobility and the lack of need of those medications that once they leave the hospital, they should be able to drive.”
- Under the Rapid Recovery Protocol 2.0, select patients can drive their cars five days after surgery if they are not taking any medications.
- To further enhance the Rapid Recovery Protocol 2.0, Dr. Gerdisch has implemented several optimizations including anemia protocols, smoking cessation support, exercise protocols, resistive breathing, nutrition support (e.g. carbohydrate loading, amino acids) and respiration therapy.
- Use of extended care facilities for elderly, frail and complex patients has significantly decreased under the Rapid Recovery Protocol 2.0 from 30% to 10%. “The extended care facilities are wonderful places, wonderful people staffing them, working for those patients, taking care of them, doing their rehab,” states Dr. Gerdisch. “But, people want to go home. So, we’ve gone from 30% of patients, a complex patient population, going to some type of extended care facility, discharged to some type of rehab, down to less than 10%.”
- Dr. Gerdisch believes that the Rapid Recovery Protocol 2.0 has created a convergence between minimally-invasive and open chest surgery patients. “What we’ve achieved over the last several years really is a convergence between our minimally invasive surgery patients and our open chest surgery patients so that the experience is very similar,” states Dr. Gerdisch. “Whether they’re having a little incision or a full incision, the experience is very close to the same with rapid recovery and restoration of full activity.”
The Impact of Rapid Recovery Protocol 2.0?
Here is a quick video that shows the results of the Rapid Recovery Protocol 2.0 for four of Dr. Gerdisch’s cardiac surgery patients.
Many Thanks to Dr. Gerdisch & Franciscan Health!
On behalf of our entire patient community, many thanks to Dr. Gerdisch for sharing his clinical experiences and research with our community! Also, many thanks to the Franciscan Health team for taking such great care of heart valve patients.
Related links:
- Surgeon Insights: Minimally-Invasive Mitral Valve Repair Surgery
- Dr. Gerdisch Interview: The Different Faces of Mitral Valve Disease
- See 100+ Patient Reviews for Dr. Gerdisch
Keep on tickin!
Adam
P.S. For the deaf and hard of hearing members of our community, I have provided a written transcript of the video with Dr. Gerdisch below.
Video Transcript:
Dr. Gerdisch: My name is Mark Gerdisch. I am chief of cardiothoracic surgery at Franciscan Health in Indianapolis, Indiana.
We started a very aggressive program of patient recovery that expedited getting out of the hospital, getting back to your life, being fully active. Our staff enjoys it, the nursing staff, respiratory therapy, physical therapy. We get to see how it influences the patient from before surgery all the way through their complete recovery. We watch that time getting condensed, the experience getting better, and patients are – they’re very vocal about it. They can’t believe that they’ve gotten to this stage so quickly.
Dr. Gerdisch: During the last five years, the heart surgery recovery process has changed a great deal. Several years ago, we initiated a very aggressive program for rapid recovery. It was really borne out of, first, recognizing that the folks for whom we did minimally invasive surgery, were feeling well and mostly pain-free, and getting out of the hospital really quickly.
We wanted it to be the same for the people for whom we did sternotomy. We just wanted them to have the same experience.
The first thing we did, that foundational building block, was to move toward everyone having rigid plate fixation of the sternum. Everybody has an orthopedic repair of the bone, the divided bone, so that we take the bone out of the equation. Recognizing that we could give them their mobility, we also saw their pain go way down, to the point where we reduced the use of opioids by 96%.
Now we knew, we’ve got dramatic pain reduction. How do we optimize the experience for the patient, recognizing that they’re no longer burdened mostly by the use of opioids? What happened, then, was we started to diminish the amount of medication that was used in the operating room so that people could get extubated in the operating room. More and more patients come out of the operating room, no matter what the approach is, or already off the ventilator.
They’re comfortable. They can be off the ventilator. They can breathe. Then within four hours, the patient gets up out of bed. What it does is it lets them recognize they have not been disabled by the operation.
Next day, up in the morning, nobody gets back in bed all day; they’re up walking. All that is achieved not only because we’ve done rigid sternal fixation and because we’ve decreased the need for those medications, but we take this very global approach, first, to pain, which includes when the patient comes into the operating room, everybody gets an erector spinae block.
The anesthesiologist, it takes him ten minutes, he puts some medicine in your back, and it gives you this general sense of comfort for the musculoskeletal system of the chest.
They get the rigid sternal fixation, then they get minimal opioids, they get off the ventilator quickly. They’re moving because we’ve let them use their arms. What we’ve gone to now is almost no restrictions. Day after surgery, up to 15 pounds in each arm. Basically, over the next few weeks we let you get up to 25 pounds in each arm.
The other thing that we recognized was that with that mobility and the lack of need of those medications that once they leave the hospital, they should be able to drive. What we did was first we said ten days, then we said a week, and now we’re at five days. Five days after you leave the hospital, you can drive. If you’re not taking any pain medicine and you’re not having a visiting home nurse, you can drive when you leave the hospital.
This gets into this global perspective of how do we optimize everything so that everybody gets that experience? Then we backed up. We backed up to when we first meet the patient, and we started to become very rigorous about anemia protocols, making sure that somebody’s hemoglobin was normal when they had heart surgery.
We have a great team of hematologists who participate with us, who in the preparation for the patient makes sure the hemoglobin’s normal. We get rid of the transfusion.
Stopping smoking, smoking cessation, we work with them ahead of time for that. Prehab, we have a process where if somebody – there’s data on this; this has been published. If someone is deconditioned before going into the surgery, then we try to get them rehab, which really is prehab, before they go into the hospital.
We have an exercise protocol. If we don’t have a means to actually engage them with a rehab professional, we give them exercise protocols to do at home and they do them.
We also give them resistive breathing devices so they can work on the strength of breathing coming in. That’s good for people who are weak. It’s also really good for people who are strong. They come in – people come in energized. Their musculature is ready for everything that they need to do.
We address nutrition up front as well. People are front-end loaded with the amino acids and things that they need. We have a special drink that they need to heal well. Then we carb-load them right before surgery. People hear of carb-loading before running a marathon. You’re about the run a marathon. You’re having a heart surgery. We carb-load them coming in. This, of course, means then that we have to tighten up their glucose control around the time of surgery, which we always do. It’s super effective because it’s starts with anesthesia and moves onto the floor with our nurses and with our endocrinologist. We have endocrinologists that see every patient, even if you don’t have a history of diabetes, because we want to control those blood sugars. We want to optimize how you’re metabolizing the blood sugar and how you’re using the nutrients in your body.
Respiratory therapists are going to be working with your breathing. We get them energized about that. They come to the hospital ready.
We’ve shortened the post-op after you leave recovery process. Now, people are driving; they’re going to the store; they’re going to church; they’re going to see their friends; they’re spending time with their families in a normal fashion. Being able to operate on somebody and have them – even with a sternotomy, let alone minimally invasive, and have them be able to go to their daughter’s wedding a week later. That’s a really beautiful thing. We’ve been able to achieve that.
Now, a little bit you’re thinking there, well, that’s kind of like the more healthy folks having heart surgery. Let’s look at the little bit more challenging. This becomes super important because now we’re talking about Grandpa and Grandma. We’re talking about folks who have multiple comorbidities that have issues that limit them in their life. We have found that applying these same principles has dramatically improved their recovery as well.
The way we measured that was we looked at – before we started this, looking back at 2015. Then we looked at 2017, ’19, ’21. What we see is that we’ve had a steady decrease in the patients that go to extended care facilities. This, I think is our greatest badge of honor. People don’t want to go to those places. The extended care facilities are wonderful places, wonderful people staffing them, working for those patients, taking care of them, doing their rehab. People want to go home. So we’ve gone from 30% of patients, again, a complex patient population, going to some type of extended care facility, discharged to some type of rehab, down to less than 10%.
Think of that in terms of days at home. That’s what we’re after. Somebody said to me, “Well, you must be having a lot of readmissions then because you’re sending people home,” so we looked at it. As it turns out, our 30-day readmission is single digits. Anything below 10% for 30-day readmission is good. We hover right around 6 or 7%.
Dr. Gerdisch: What we’ve achieved over the last several years really is a convergence between our minimally invasive surgery patients and our open chest surgery patients so that the experience is very similar. Whether they’re having a little incision or a full incision, the experience is very close to the same with rapid recovery and restoration of full activity.