Ari’s Patient Success Story: The Value of Shared Decision-Making for Patients & Surgeons
Written By: Adam Pick, Patient Advocate & Author
Medical Expert: Eric Roselli, MD, Adult Chief of Cardiac Surgery, Cleveland Clinic
Published: August 2, 2022
Thirty years after meeting on a football field at the University of Michigan, the friendship of Ari Mintzer and Dr. Eric Roselli took an interesting turn.
Ari, an attorney from Highland Park, Illinois, needed help. His first aortic valve replacement, implanted in 2007, was failing. He was short of breath. Ari needed another heart surgery. During his search for answers, Ari called Dr. Eric Roselli, his old friend, who was now the Chief of Adult Cardiac Surgery at the Cleveland Clinic and an aortic valve specialist.
This is the story of Ari and Dr. Roselli, their friendship, and their shared-decision making processes as patient and surgeon.
Key Learnings From Ari’s Patient Success Story
Here are important insights specific to Ari’s story, the lifetime management of heart valve disease and shared decision-making opportunities:
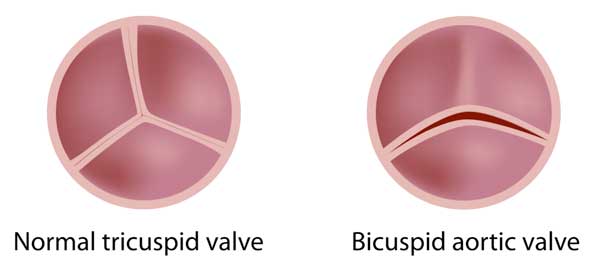
- Ari was born with a bicuspid aortic valve that required a surgical aortic valve replacement (SAVR) and an aortic aneurysm repair in 2007. Ari selected a cow (bovine) valve replacement knowing that in the future he would need another operation. Most tissue valves – cow valves or pig valves – last between 10 to 15 years.
- Following his initial SAVR, Ari had no health issues for the next 13 years until the cow valve began to fail. Ari became symptomatic and began to feel short of breath upon exertion.
- According to Dr. Roselli, the diagnosis of a bicuspid aortic valve and an aortic aneurysm is very common among his patients. “We know that close to 2% of the population is born with an abnormal aortic valve. It gets broadly categorized as bicuspid aortic valve but there’s a real spectrum of how that congenital abnormality presents in different people,” states Dr. Roselli. “We have patients that range from infancy to their 80s. A lot of patients had aneurysms associated with the valve dysfunction.”

- Using a shared decision-making approach, Ari and Dr. Roselli developed a unique 50-year strategy for Ari’s lifetime management of heart valve disease.
- While a mechanical valve replacement may have provided Ari a lifetime solution, given the potential long-term durability of mechanical valves, Ari is very active and did not want to be on blood thinners (e.g. warfarin) for the rest of his life.
- To avoid another incision to his chest, Ari considered a transcatheter aortic valve replacement (TAVR). However, the durability of TAVR, using a Valve-in-Valve approach, was questionable given the lack of research, data and outcomes for younger patients.
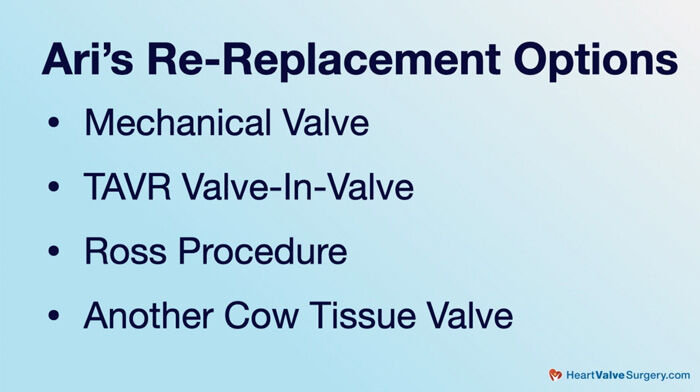
- Ari and Dr. Roselli also considered the Ross Procedure. Ari states, “I was dead set on going with the Ross Procedure for a period of time. It just was one of those things where, at the end of the day, there was a potential risk of creating another valve problem on the pulmonary side.” Reflecting on the possibility of a Ross Procedure for Ari, Dr. Roselli states, “I’m a little stricter about who I do Ross Procedures on. In Ari’s particular situation, he’s already had his aortic root and his ascending aorta replaced. It didn’t make sense to do a Ross Procedure as the redo in a guy who had a history of aortopathy whose valve was degenerated.”
- After many conversations, Ari and Dr. Roselli collectively felt a second SAVR was the best option for Ari’s next procedure. Ari states, “I had surgical aortic valve re-replacement with another cow tissue valve. We went with a bigger valve this time so that we could do a Valve-in-Valve down the road.”

- According to Dr. Roselli, “shared decision-making” is an important topic right now. Dr. Roselli states, “It’s kind of a buzzword topic these days. I’m glad because in the current world of healthcare where you have really a really broad spectrum of decisions to make, which is nice, but also can be very confusing. In the end of the 1800s, it was considered ethically wrong for a patient to not listen to their doctor. We don’t live in that kind of world now. It’s great that we don’t because there’s knowledge everywhere for everybody. I love it when a patient comes in with one of those yellow legal pads full of questions. Even physicians have these guidelines. It’s a guideline. For any individual patient, your decision should be personal. They should be tailored to all of your medical specifics and your personal desires as well as the expertise of that physician you’re working with. To me, that’s what shared decision-making means. I think everybody does better when we embrace this concept.”
- Ari’s advice to patients is to gather as much knowledge as possible about your disease, your medical team and your treatment options. “It starts with knowledge. I know it’s cliché. Knowledge is power. But it really is, especially in this world,” states Ari.
- Dr. Roselli’s advice to patients complements Ari’s point about knowledge. “Knowledge is power. The reason is because fear comes from the unknown. I have seen this over and over again where I meet with a patient. I can tell sometimes they don’t know how to ask the right questions. But, I can tell they don’t understand the situation. I think it’s our responsibility to make sure that when we leave the office, the patient understands enough that they feel comfortable with the decisions they’ve made. Sometimes it means drawing a picture or finding some way to communicate with them and make sure that their questions are answered.”
Many Thanks to Ari, Dr. Roselli and Cleveland Clinic
On behalf of our patient community, many thanks to Ari and Dr. Roselli for sharing their fantastic story with us. We also want to thank the entire Cleveland Clinic team for taking such great care of patients with heart valve disease.
Related Links:
- See Dr. Eric Roselli’s Interactive Surgeon Profile
- Heart Surgery Innovations: Bicuspid Aortic Valve & Aortic Aneurysms with Dr. Eric Roselli
- Explore the Cleveland Clinic Heart Valve Microsite
Keep on tickin!
Adam
P.S. I didn’t mention it above… But, I attended the University of Michigan at the same time as Ari and Dr. Roselli. In fact, the three of us were in the same fraternity, Sigma Alpha Mu, and Dr. Roselli was my “Big Brother” in that fraternity. I can not be more happy and more thankful knowing that Ari’s heart is doing great thanks to Dr. Roselli.
P.P.S. I have provided a written transcript of this video interview below for the the deaf and hard of hearing members of our community.
Video Transcript:
Adam: Hi, everybody. It’s Adam with heartvalvesurgery.com. This is a very special video about shared decision-making between patients and their surgeons. I am thrilled to be joined by Dr. Eric Roselli who is the chief of adult cardiac surgery at the Cleveland Clinic in Cleveland, Ohio. During his extraordinary career, Dr. Roselli has performed thousands of heart valve repairs and heart valve replacement procedures. We are also joined today by a two-time heart valve surgery patient, Ari Mintzer from Chicago, Illinois, who is one of Dr. Roselli’s patients. Dr. Roselli, it is great to see you again. Thanks for being on the line.
Dr. Roselli: Hi, Adam. Always great to see you, too, man.
Adam: Yeah, and we also have with us Ari Mintzer. Ari, thanks for being with us today.
Ari: Thanks for having me.
Adam: Yeah, so we’re going to get into this topic of shared decision-making, but first, I understand, Ari and Dr. Roselli, that you two have a little bit of a history together. Ari, maybe you can share with all the viewers how you first came across the name Eric Roselli.
Ari: Sure, so I was at the University of Michigan back in 1992 pledging Sigma Alpha Mu fraternity. Eric at that time was a senior. We actually first met on the intramural football field. I’ve known him ever since.
Adam: I guess you’d say a little cherry on the top is that I was very fortunate to be in Ann Arbor at the University of Michigan at the same time as the two of you. This really is a wonderful reunion of sorts, except we’re not talking about Michigan football. We’re talking about heart valve surgery. Let’s get into that. Ari, for the patients who maybe don’t know your story, can you share a little bit about your history? What were you diagnosed with and what was your original treatment?
Ari: Sure, so I was born with a congenital heart defect. My aortic valve was bicuspid as opposed to tricuspid. Aortic stenosis insufficiency was the way they described it to me. I was monitored that for the better part of my first 30-some odd years of living, but about 15 years ago, it was time to get the valve replaced. I had a surgical aortic valve replacement with a cow tissue valve and an aneurysm repair. I had done that here locally in Chicago.
Adam: Ari, you had the initial SAVR aortic valve replacement. Can you talk about how that worked for you?
Ari: Once you get past that initial phase of getting out of the battle of the open-heart surgery, everything was unbelievable. I mean, I felt like I’d never felt before. I had an extra breath to me. I could run long distances without being extremely fatigued. Any sport I wanted to play, there really were no limitations, whereas previous to the surgery, I was constantly getting winded and reminded of the fact that I had a medical condition.
Adam: Ari, it’s great to hear about that result. How long did that continue for?
Ari: The good times lasted for probably about a decade. Then give or take around ten years, I started to feel myself getting a little bit more tired with the same level of activity. I chalked it up to just aging as opposed to anything wrong with the valve. I would say probably about, I said 10, probably like 12 years I felt pretty good, and again, didn’t even think about the fact that I was going to have to have my valve replaced once again.
Adam: Then came the news, right? I’m guessing you’re feeling some fatigue, out of breath. You go see a doctor, have an echo. What did you learn?
Ari: Sure enough, the valve that had been replaced, its time had come and so the decision process began of, okay, now what do we do?
Adam: Dr. Roselli, you see a lot of patients, thousands of patients at the Cleveland Clinic. Is the scenario that Ari just shared with us common?
Dr. Roselli: Yeah, absolutely. We know that close to 2% of the population is born with an abnormal aortic valve. It gets broadly categorized as bicuspid aortic valve but there’s a real spectrum of how that congenital abnormality presents in different people. We have patients that range from infancy to their 80s. A lot of patients had aneurysms associated with the valve dysfunction. Some of the valves leak. Some of the valves are stenotic. There’s a whole bunch of details about the disease that are important to understand.
Adam: Ari, it’s obvious you got in touch with Dr. Roselli to help you out, but I’m curious to know. Why specifically did you want to hear from Eric about his thoughts on your valvular condition?
Ari: First and foremost, you want to go with people that you know and you trust. That was the obvious connection there, not to mention that Eric is one of the top performers at one of the top places in the world. It just seemed this is who you want to speak to. Eric was very clear on you’ve got lots of different options to choose from these days. We just walked through all those potential options at that time. At that point, it was time to do my homework and to really go out there and pursue those different avenues and figure out what’s going to be the best solution for me given my lifestyle, given my age, given what I want to accomplish in this lifetime. What is going to make the most sense? It was great to have Eric as that sound initial sounding board to present me with all the various different options that were out there.
Adam: Eric, you get the phone call from Ari, known him for 30 years. I’m curious to know. From a surgeon perspective when you hear him talk about his aortic valve, it’s failing, the aneurysm that was already replaced, where does your mind go in terms of how you might be able to help him?
Dr. Roselli: We consider it a privilege when people ask for our help. When it’s a friend that I’ve known, Ari has known me before I was Dr. Roselli, calls and asks my advice about something, I’m like this is the best thing ever. I’ve got a friend that’s asking me about help and it’s in my wheelhouse. That’s the first thing. I think I was driving in my car when we were talking about this the first time around, Ari. I told you I’m going to tell you because you’re my friend the straight thing, but then after I said that, I thought I’m always this way with my patients. Because it’s not an easy decision. It’s never an easy decision about what to do and how to do it. It’s also scary when you’re in this situation and you have all these choices to make, but it sure is nice to be able to sit down and think through it versus being swooped up on a helicopter and brought somewhere where you have to have something done in an emergency.
Adam: Ari, Eric, this is just an open question for you both. Maybe we’ll start with Ari. It’s 2022. It’s not 1962. There are options for aortic valve reoperations all over the place. I’m curious to know. What was your thought process, what did you consider, and ultimately, what did you guys choose together?
Ari: Yeah, for me, the decision came down to did I want to be looking at a mechanical valve. That was a quick no. The idea of being on a blood thinner for the rest of my life, having to worry about some of the other – the ticking that goes along that I heard about, the potential for aneurysms and strokes, it was just too much for me. I have a very active lifestyle. I have three boys, two dogs, and a wife. We like to be outdoors. We like to be playing sports and running around doing stuff. That was not a viable option.
The second option I considered was the TAVR. There were great things about that that I’d heard about. You’re in and out within a day. Everything is great, right? You don’t have to have your chest cracked open. There’s a lot of benefits. The problem was my age demographic, there wasn’t a lot of history. There still isn’t a lot of history and data on longevity.
I then looked into the Ross procedure. Eric and I talked about that a great length along with the others. I was dead set on going with the Ross procedure for a period of time. It just was one of those things where, at the end of the day, there was a potential risk of creating another valve problem on the pulmonary side down the road. I just felt like, for me, that was too big of a risk. I had surgical aortic valve re-replacement with another cow tissue valve. We were going to do a bigger valve this time so that we could down the road do another valve within valve. That was it.
Adam: From your perspective, Eric, what were you thinking when it came time for that surgical aortic valve replacement?
Dr. Roselli: Ari said it very well. The valve in valve option at this point, although we know it can be performed pretty safely, it’s really unclear how durable that is. For somebody who we know is going to outlive another biologic valve, whether it’s TAVR or SAVR, I trust the surgical valve better because I have good data. That technology has been pretty stable in the design dating back to the ‘80s. We have decades of follow-up data on thousands of patients.
Ross, I do Ross procedures. I’m a little stricter about who I do Ross procedures in. In my experience, it is younger patients, typically 40 or younger, sometimes in their 40s, but in Ari’s particular situation, he’s already had this root and his ascending aorta replaced. The reason was in his 30s that he already had evidence of aortopathy or aneurysm of his aorta. When you’re born and when you’re developing in utero, the cells that become your aorta also are the same cells that become your pulmonary artery. If we take that pulmonary artery and put it in the aortic position under those load conditions on the left side of the heart, there’s a risk that Ross could fail by causing an aneurysm in you. It didn’t make sense to do a Ross as the redo in a guy who had a history of aortopathy whose valve was degenerated. It made more sense just to get you a new valve. I thought that a lot of our discussions focused on mechanical versus biologic.
Adam: Eric, great learning all of this information, which I didn’t know, and Ari, thank you for walking us through how you went about the steps to choose the surgical aortic valve re-replacement. One thing that I got from hearing you two talk is this decision-making process. In cardiac surgery right now, the idea of shared decision-making is big among patients and their medical teams. To start, Eric, can you maybe help the patients understand exactly what is shared decision-making?
Dr. Roselli: It’s kind of a buzzword topic these days, shared decision-making. I’m glad because in the current world of healthcare where you have really a really broad spectrum of decisions to make, which is nice, but also can be very confusing, talking about this concept of shared decision-making forces us to slow down and make sure that we’re doing exactly that. A couple of generations ago, physicians were very paternalistic. In fact, in the end of the 1800s, it was considered ethically wrong for a patient to not listen to their doctor. We don’t live in that kind of world now. It’s great that we don’t because there’s knowledge everywhere for everybody.
I love it when a patient comes in with one of those yellow legal pads full of questions. Bring it. Let’s talk about it. Let’s make sure that all the knowledge that you’re getting is being interpreted well and being brought into the very specific personalized perspective of your issue. That’s where your doctor can help you because you’re going to get information from a whole bunch of different places. Even physicians have these guidelines, documents. It’s a guideline. For any individual patient, your decision should be personal. They should be tailored to all of your medical specifics and your personal desires as well as the expertise of that physician you’re working with. To me, that’s what shared decision-making means. I think everybody does better when we embrace this concept.
Adam: Dr. Roselli, I loved hearing your explanation and description of shared decision-making. I also loved hearing about those patients who are coming in with all of those notes on that yellow legal pad saying let’s figure this out together. I’m curious to know. When you think about the lifetime management of valve disease for your patients today versus 15 years ago, is this conversation more wanted because we’re living life longer, we’re learning that perhaps early surgery for things like valvular disease is a good thing, not a bad thing? Can you talk about the lifetime management and how that might correlate to shared decision-making?
Dr. Roselli: I love that. I teach all my residents and med students and fellows and everything else, even when we do research projects, let’s not focus on the thing that we’re doing, the procedure we’re offering. Let’s focus on the disease that we’re treating, start from that base and give it that broad view. Because it’s a fast-moving train. This is a moving target and all the objectives that we want now may be different than they were five or ten years ago. The tools in the box have changed. We have to appreciate that and do the best we can to look down the road.
For example, in the valve space, if I’m going to put a bio prosthesis in a young guy like Ari Mintzer who’s going to outlive that valve, maybe outlive a couple of them, I’m going to make sure it’s big enough that it not only is very efficient and can allow him to exercise and do all the things he wants to do, it’s also going to be efficient which may translate to being more durable, which is pretty cool. Also, it’s going to be big enough to house a TAVR valve in the future as that technology evolves and we gather more data in the next decade and understand that that might be a real option for him. I also make sure little details, like how I sew that valve in, that if I have to come back and operate again, it’ll be easy for me to cut it out in such a way that I can drop another one in without having to take the whole aorta all apart. There’s all those little details that we keep in mind with that broad view of lifelong care.
Adam: Eric, loved hearing that, and going right over to Ari. When you were going through this decision-making process, you and I had several great calls talking about what was available to you. I remember one of the first things you said to me was, “Adam, I just want to figure out a way to get to 90.” In my head, I struggled with how we were going to do that because at the time you were thinking about TAVR and I was kind of I don’t know. I’m curious to know. Given all of this discussion about your options, all of the physicians you talked with, talking with Dr. Roselli, do you feel like this shared decision-making approach has got you to that path to ninety.
Ari: Absolutely, yeah, no, it’s funny because I go back in my head, too. Eric and I talked about it extensively, too, was if you did this and then that and then the other, this would get you to 80, or if you did this way and that way and the other, this could get you to 75 before you have to get a reoperation. We went through all the math and all the numbers. That was just out there in terms of, okay, we know there needs to be something else down the road, but what’s the most viable path to 90, and Eric is focusing on 100, which is great.
Adam: Ari, you have, no doubt, been through a lot when it comes to your heart, your heart valves, the aorta replacement. I imagine patients are really enjoying this conversation. They might be wondering what advice might you have for someone who is in maybe a similar situation or maybe is in just a different valvular condition, maybe something with their mitral valve. What advice would you have for them about developing shared decision-making approach with your medical team?
Ari: It starts with knowledge. I know it’s cliché. Knowledge is power, but it really is, especially in this world where, look, I have to imagine most of us who are heading into this, we have a different day job, right? We’re not in the medical field. While it’s probably a small deal for something, even open-heart surgery for Eric to perform because he does it every day, for the patient, it’s a big deal. Like anything, for me at least, and what I would recommend to everyone, is just there’s a significant amount of information out there, different resources, whether it’s online or books or anecdotally or other patients, right? Just to get as much information and knowledge as possible so that you can ask the right questions.
Because a lot of times you don’t know you don’t know. If you just go out there and be a sponge, act as if you’re a sponge, take in everything, appreciate how it relates to you, and then really make your – the yellow notepad you talked about earlier, really write everything down so that you can walk into a doctor’s office or give a call to Eric and say, “Hey, these are the questions that I have. These are the options I’m thinking about. What am I missing? What are the benefits? What are the risks?” Really going through that process I think it’s critical having that knowledge.
Adam: Ari, I’ve got to give you a lot of credit because I remember how hard you went at this trying to learn as much as you can. Now let’s flip it over to Eric from the surgeon’s perspective. It’s one thing to say let’s go do our research, let’s go figure out what we think is right, but when we get into that office and maybe the patients are a little nervous or they have whitecoat anxiety, what advice would you have for patients or maybe what do you do to help a patient feel like they can be part of the shared decision-making process.
Dr. Roselli: Yeah, look, you said knowledge is power. The reason is because fear comes from the unknown. I have seen this over and over again where I meet with a patient and I can tell sometimes they don’t know how to ask the right questions but I can tell they don’t understand the situation. I think it’s our responsibility to make sure that when we leave the office, the patient understands enough that they feel comfortable with the decisions they’ve made. Sometimes it means drawing a picture or finding some way to communicate with them and make sure that their questions are answered.
We pay a lot of attention to that in the medical field to make sure that we’re good about addressing that. Because people come with all different kinds of backgrounds and knowledge and communicate in different ways. I tell you. It’s always satisfying to me when someone comes in, I can tell they’re afraid, and we get to a point of knowledge or at least comfort with a decision and I can see the furrow in their brow relaxes and they’re at ease. Even if it’s a bad situation or a tough situation, people are courageous and they can handle it. I think that’s important for us to make sure that we’re addressing it that way.
Adam: Ari and Eric, loved hearing about your views on shared decision-making. Really what I heard from both of you is what I really hope patients can embrace, which is, Ari, that knowledge is power, that’s the education. Eric, I loved how you really take a patient-specific view for tailoring their treatments and empowering them to ask the questions they need answered, not just for the now but thinking about what might happen given the nature of valve disease over their lifetime. On behalf of all the patients at heartvalvesurgery.com, anybody watching this video, I want to thank you for being with me today and sharing your thoughts on shared decision-making. Thanks for being here.
Ari: Thanks, and first and foremost, thanks to Eric for all he’s done for me. I don’t have enough words out there. Thanks for everything. Adam, thanks for all that you’re doing for the heart valve community. Really greatly appreciate it, I’m sure, by everyone all around the world.
Dr. Roselli: Thanks for putting your trust in us, Ari. Keep up the good work, man. You too, Adam. Thanks for the opportunity to empower patients. Really great discussion today, guys. Thanks.






