Surgeon Q&A: Patient Candidacy for Robotic Mitral Valve Surgery
Written By: Allison DeMajistre, BSN, RN, CCRN
Medical Expert: Husam Balkhy, MD, Director of Robotic Cardiac Surgery, University of Chicago Medicine
Reviewed By: Adam Pick, Patient Advocate, Author & Website Founder
Published: September 22, 2025
Since the first robotic mitral valve repair surgery was performed in 1998, cardiac surgeons have continued to develop and master robot-assisted techniques to treat patients with heart valve disease. However, not every patient is a candidate for robotic heart surgery.
To learn more about patient candidacy for robotic mitral valve surgery, we interviewed Dr. Husam Balkhy, a world-renowned cardiac surgeon at the University of Chicago Medicine. During his extraordinary career, Dr. Balkhy has performed over 2,500 robotic surgeries.
Dr. Balkhy Explains the Facts About Robotic Mitral Valve Surgery
Here are the key insights Dr. Balkhy shared in this interview:
- What is your history and experience with robotic mitral valve repair? How many procedures have you performed? Are robotics a big part of your practice? “It has become a much larger part of my practice than before,” said Dr. Balkhy. “I started doing robotic heart surgery in 2006, so we’re closing in on 20 years now. I do all manner of robotic surgery on the heart coronaries, valves, ASDs, congenital diseases, and tumors of the heart. My whole practice is focused on robotic heart surgery. I don’t do any open surgery at all anymore, which is a luxury. It’s also a huge benefit to the patients, and our program is sought out from all over the world for robotic heart surgery. In terms of the mitral valve specifically, I would say about 60 percent of my robotic heart surgery volume is now mitral valve. We’re closing in on about 900 or so robotic mitral valve procedures. We’ve gotten very good at identifying who’s a candidate, who’s not a candidate, and making the outcomes as best as they can be.”
- What is the value of the robot for both patients and surgeons? “That’s a great question,” said Dr. Balkhy. “I just finished clinic about a half hour ago, and I’ve had that conversation recently. One of the benefits to the patient is that we can see the mitral valve better than what can be seen through a sternotomy. The only people who recognize this fact are surgeons who are using the robot because the mitral valve is positioned such that it faces the right chest. So, when I insert my robotic camera, which is 10 to 12 times magnified, very clear 3D, the Da Vinci robot is now in its fifth generation. So, it is a highly well-oiled machine, and it’s just a beautiful view. I can see the mitral valve with all of its structures and all of the components of it. In my own experience, the view is 100 times better than I could see when I was cracking the chest open because I had to rotate the valve facing to the right to allow it to face the top. There are good studies with data that show patients who have their mitral valve approached through the side with a scope have a higher likelihood of repair. As most of your patients probably know, as you’ve educated them nicely over the years, a repair is much better than a replacement. So that’s a huge benefit from the patient standpoint.”

- Robotic surgery allows for a quicker recovery. “The second benefit is that you don’t have a sternotomy, which means you don’t have to heal from a sternotomy,” said Dr. Balkhy. “We find that the less invasive the approach, the quicker the recovery. When we do robotic mitral surgery in my program, we are doing it endoscopically. The largest incision the patient has measures eight millimeters in diameter. So, once the chest tubes are out, which usually happens the next day, they don’t have any pain and don’t require narcotic pain medication. It’s not uncommon for our healthy, young patients with mitral valve disease who get a repair to go home the next day. If they have a job that requires them to be back in the office, they’re back within a couple of weeks, and a physical job is within two or three weeks. There’s no restriction that I impose on my patients. It’s more just when the soreness is better.”
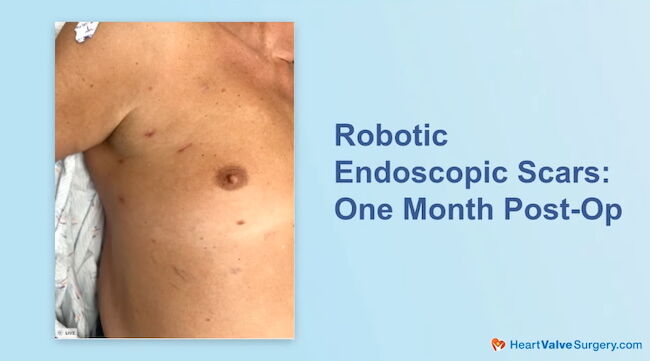
- Pain is minimal with robotic surgery and narcotics pain medicine is often not used by patients. “We did a study on postoperative pain management, and we found that almost 80 percent of our patients never even fill the prescription for narcotic pain pills we send them home with. So, once the chest tubes are out, they stop taking anything narcotic.”
- There are benefits of robotic surgery for the surgeons as well. “The ergonomics of the surgeon are significantly better when we are sitting down and able to conduct the operation in a more comfortable position,” said Dr. Balkhy.
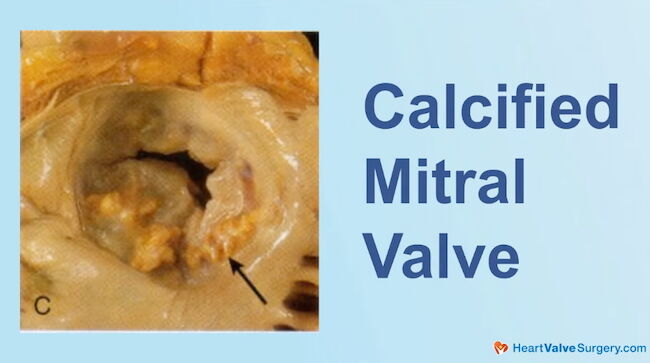
- Who is a good candidate for robotics? “I think that is closely aligned with the surgeon and the surgical team’s experience,” said Dr. Balkhy. “As we get more experienced in robotic surgery, the inclusion criteria open up a bit, and I’ll explain what that means. When I first started doing robotic mitral surgery, I was focusing only on patients who had isolated mitral valve disease. We didn’t do those if they had an accompanying tricuspid valve problem. We wouldn’t do those if they had a complex valve or a previous operation. That’s all changed very quickly. Within the first four or five years, we gained a lot of experience. Now, the exclusion criteria are very minimal. The only patient I would shy away from now is somebody who has a heavily calcified valve that would do better with decalcification using the traditional approach. But, even in those cases, we have a lot of new things that can be applied from the side using a robotic approach, so even that is not a strict contraindication.” Dr. Balkhy explained that patients who have had previous heart surgery through a sternotomy and those with previous mitral valve surgery through the side using a robotic approach or a non-robotic mini-thoracotomy approach are all candidates for robotic surgery.
- Is there a patient that would not be a candidate for robotic surgery? Dr. Balkhy explained that a patient who would not be a likely candidate for robotic surgery is someone who has had a lung resection. “If somebody had previous lung resection surgery, and I’m talking major resection, the likelihood that there is not a lot of scar tissue in their chest is pretty low. Those are the patients we step away from, and we suggest they would be better served with a sternotomy incision. But regular scar tissue from previous heart surgery we would do.”\
- Many patients have comorbidities like atrial fibrillation and coronary artery disease. Can the robot treat those cardiac conditions and mitral valve disease? “Absolutely,” said Dr. Balkhy. “I’ll take atrial fibrillation first. That is a very common association with mitral valve disease. We see a lot of it, and the approach is the same as what we would do for isolated mitral valve repair. We do the Cox Maze operation, which is very effective. We use the robot to treat atrial fibrillation by itself, sometimes called standalone AFib. It’s a less invasive operation with little holes from the right side. We can do the same thing in combination with the mitral valve. Now, if someone has coronary artery disease, I think it was in 2010 when I was first faced with this problem. We did a combined robotic, totally endoscopic coronary artery bypass and mitral valve repair. I think we have a couple of those this month. It entails expertise with robotic TECAB as well as robotic mitral valve repair. We select those patients very carefully. We wouldn’t do the surgery on someone who needs a triple bypass and a mitral valve. Instead, it’s usually someone with single or double vessel coronary disease, and we would combine them.”
- Can a mitral valve and an aortic valve procedure be performed at the same time? Dr. Balkhy said, “A combination of aortic valve and mitral valve problems can also be managed robotically. We have some good publications and videos on that topic in terms of teaching. However, we need to choose those patients carefully. They have to be robust with good left ventricular function.” Dr. Balkhy added that the surgeon needs to know precisely what they are doing.
- Are there any misconceptions about robotic mitral valve surgery? “One misconception I see a lot, and I talked about it in my clinic today, has to do with patients who require a mitral valve replacement. It is a misconception that those patients cannot have a robotic operation, which is not true. Those are sometimes easier than repairs. I saw a young woman today with rheumatic heart disease who has a stiff valve that we would normally not have success repairing, so we are going to replace her valve robotically. The largest incision will be the size required to put the valve inside the chest, but that’s it. Everything else is eight millimeters. So, I think there are very few patients today that I would not operate on with the robot.”
Thanks Dr. Balkhy and the University of Chicago Medicine!
On behalf of all the patients in our community, many thanks to Dr. Husam Balkhy, for everything you and your team are doing at the University of Chicago Medicine in Chicago, Illinois!
Related links:
- Dr. Husam Balkhy Q&A: Coronary Artery Disease & Heart Valve Disorders
- Robotic Mitral Valve Surgery Patient Education Center
- See More Than 50 Patient Reviews for Dr. Husam Balkhy
Keep on tickin,
Adam
P.S. For the deaf and hard-of-hearing members of our patient community, we have provided a written transcript of our interview with Dr. Balkhy below.
Video Transcript:
Adam Pick: Hi, everybody. It’s Adam with heart valve surgery dot com. And this is a special surgeon question and answer session all about patient candidacy for robotic mitral valve surgery. I am thrilled to be joined by Dr. Husam Balkhy, who is a leading cardiac surgeon with a super specialty in robotic mitral valve surgery at the University of Chicago Medicine in Chicago, Illinois.
Dr. Balkhy. It is great to see you again. And thanks for being with me today.
Dr. Husam Balkhy: Thank you, Adam. Great to see you again as well.
Adam Pick: Dr. Balkhy, we’re going to talk all about your specialty in robotics, but first I want to thank you for being a long, long time supporter of HeartValveSurgery.com.
We’ve known each other for over 15 years. We’ve filmed several videos together educating patients and last I checked, you have successfully treated over 75 patients in our community. So, thanks so much to everything you and your team are doing to help our patients.
Dr. Husam Balkhy: Thank you. I appreciate that Adam and and yes, we’ve known each other for uh for 15 years now and I’m a big fan of what you’re doing.
I think it’s a great service to our patients that are interested in learning about valve surgery. And I hear your name a lot. The website is frequented very much by our patients. So, so thank you as well.
Adam Pick: Let’s keep that momentum going and now let’s talk about Patient candidacy for robotics. Can we maybe start by learning a little bit about your history and your experience with robotic mitral valve surgery? How many procedures have you performed and is it a big part of your practice?
Dr. Husam Balkhy: Absolutely. It has become a much, much larger part of my practice than before. I started doing robotic heart surgery in 2006.
So we’re closing in on 20 years now. I do all manner of robotic surgery on the heart coronaries, valves, ASDs, congenital disease, tumors of the heart, and so, my whole practice is focused on robotic heart surgery. I don’t do any open surgery at all anymore, which is a luxury if you will, but it’s also, a huge benefit to the patients and, you know, our program is sought out from, from all over the place to have that done.
In terms of the mitral valve specifically, about I would say 60 percent of my robotic heart surgery volume is now mitral valve. We’re closing in on about 900 or so robotic mitral valve procedures. We’ve gotten very good at identifying who’s a candidate, who’s not a candidate, and making the outcomes as best as they can be.
Adam Pick: Dr. Balkhy, I can’t thank you enough for that commitment to the space of robotics. And I’ve got to ask you, I’m sure patients are wondering what is the value of the robot for both patients and for surgeons?
Dr. Husam Balkhy: Yeah, no, that’s a great question. And seeing that I just finished clinic about a half hour ago, I’ve had that conversation just very recently. One of the benefits to the patient is that we are able to see the mitral valve better. than what, what can be seen through a sternotomy.
And the only people that recognize this fact are surgeons who are using the robot. And the reason for that is the mitral valve is actually positioned such that it faces the right chest. So, when I insert my robotic camera, which, by the way, is 10 to 12 times magnified, very clear 3D, the Da Vinci robot right now is in its fifth generation. So it’s a highly, highly well-oiled machine, and it’s just a beautiful view.
I can see the mitral valve with all of its structures and all of the components of it. Almost in my mind, in my own experience, 100 times better than I was able to see it when I was cracking the chest open, because in those cases I had to rotate that valve that was facing to the right to allow it to face to the top.
And there are good studies with good data that show that patients who have their mitral valve approached through the side with a scope have a higher likelihood of repair. And as most of your patients probably know, as you’ve educated them nicely over the years, A repair is much better than a replacement.
So that’s the huge benefit from, from the patient standpoint. The second benefit is that you don’t have a sternotomy, which means that you don’t have to heal from a sternotomy and the less invasive the approach, the quicker the recovery we find. And when we do robotic mitral surgery in, in my program, we are doing it totally endoscopically.
The largest incision that the patient has measures eight millimeters in diameter. So, you can imagine how once the chest tubes are out of the chest, which usually happens the next day, they really don’t have any pain, and they don’t require any narcotic pain medicine. And so it’s not uncommon for our healthy, young patients who have mitral valve disease that get a repair, it’s not uncommon for them to go home the next day.
And if they have a job that requires them to be back in the office, they’re back there within a couple weeks and a physical job within two or three weeksvery commonly. There’s no restriction that I impose upon my patients. It’s more just when the soreness is better. We did a study on post operative pain management, and we found that almost 80 percent of our patients never even fill the narcotic pain pills that the prescription that we send them home with. So once those chest tubes are out, they stop taking anything that’s a narcotic.
The ergonomics to the surgeon are significantly better when we are sitting down, um, and able to conduct the operation in a more comfortable position.
Adam Pick: Dr. Balkhy, it’s great to hear about all of those benefits for both patients and surgeons. who is a good candidate for robotics.
Dr. Husam Balkhy: Sure. Yeah, I think that is closely aligned with the surgeon and the surgical team’s experience.
And so as we get more experienced in doing robotic surgery, the inclusion criteria open up a little bit. And I’ll explain what that means. When I first started doing robotic mitral surgery, I was focusing only on patients who had isolated mitral valve disease. If they had an, an accompanying tricuspid valve problem, we wouldn’t do those.
If they had a complex valve, we probably wouldn’t do those, or if they had a previous operation. We wouldn’t do those. That’s all changed very quickly. Within the first four or five years, we gained a lot of experience. And now, in my mind, pretty much the exclusion criteria are very, very minimal. The only patient that I would shy away from right now is probably somebody who has a really, really heavily calcified valve that would do better with decalcification using the traditional approach.
And even in those cases, we have a lot of new things that can be kind of applied from the side using a robotic approach. So even that is not a strict contraindication. But somebody say who’s had previous heart surgery through a sternotomy. Are they a candidate? Absolutely. Somebody who has had a previous mitral valve operation through the side using a robotic approach or a non robotic mini thoracotomy approach. Those are candidates as well.
There is one type of patient that would be really hard which is somebody who’s had a lung resection. So, if somebody had previous lung resection surgery, and I’m talking about a major resection, the likelihood that there is not a lot of scar in their chest is pretty low.
And so those are the ones that we kind of step away from and say you’d probably be better served with a sternotomy incision. Um, but regular scar tissue from previous heart surgery. That’s a total do
Adam Pick: Dr. Balkhy, a lot of patients at HeartValveSurgery.com have comorbidities like atrial fibrillation and coronary artery disease. Can the robot be used to treat both those cardiac conditions and mitral valve disease?
Dr. Husam Balkhy: Absolutely. Um, I’ll take atrial fibrillation first. That’s a very, very common association with mitral valve disease. We see a lot of it and the approach is exactly the same as what we would be doing for a mitral valve repair that is isolated.
We do the maze, the Cox maze operation, which is very effective. We actually use the robot to treat atrial fibrillation by itself, sometimes called standalone AFib. Uh, and that’s a nice, uh, totally less invasive operation with little holes from the right side. So, we can do the exact same thing in combination with mitral valve.
Now, if somebody has coronary artery disease, I think it was in 2010 that I was first faced with this problem and we did a combined robotic totally endoscopic coronary bypass. And mitral valve repair, and I think we have a couple of those these month this month and basically what that entails is it entails expertise with robotic T-cab as well as robotic mitral valve repair.
You have to really select those patients very carefully. Like we wouldn’t do somebody who needs a triple bypass and a mitral valve. It’s usually somebody with single or double vessel coronary disease. We would combine that.
Adam Pick: Dr. Balkhy, I’m curious, can you perform a mitral valve and an aortic valve procedure at the same time?
Dr. Husam Balkhy: A combination of aortic valve repair and aortic valve and mitral valve problems can also be managed robotically, and we have some, some good publications and videos on that topic in terms of teaching, um, and, and some of those patients can be, again, you have to choose them carefully.
They have to be robust. They have to have good left ventricular function and you have to know exactly what you’re doing.
Adam Pick: Dr. Balkhy, it’s great to hear how the inclusion criteria for robotics has expanded over the years. I’ve got to ask, are there any misconceptions about robotic mitral valve surgery?
Dr. Husam Balkhy: One misconception that I’ve seen a lot and I actually talked about it today in my clinic is patients who require a mitral valve replacement.
One of the misconceptions is that those patients cannot have a robotic operation. That’s absolutely not true. Those are actually easier sometimes than repairs. I saw a young woman today with rheumatic heart disease and she has a stiff valve that we would normally not repair with any kind of good success and we’re going to replace her valve and she’ll get it robotically.
The largest incision is going to be the size of what is required to put the valve inside the chest, but that’s it. Everything else is eight millimeters. And so I think that, um, There’s a very, very, very few patients today that I would not operate on with the robot.
Adam Pick: Well, Dr. Balkhy, I cannot thank you enough for sharing all of these insights about robotic mitral valve surgery and patient candidacy with us today. And on behalf of patients at HeartValveSurgery.com patients all over the world. Thanks so much to you and your team at the University of Chicago Medicine for taking such great care of heart valve patients. Thanks for being with me today.
Dr. Husam Balkhy: Thank you very much. Adam. It was great to be with you.





