Coronary Artery Disease & Heart Valve Disorders: What Should Patients Know?
Written By: Adam Pick, Patient Advocate & Author
Medical Expert: Husam Balkhy, MD, Director of Robotic and Minimally Invasive Cardiac Surgery, University of Chicago Medicine
Published: July 18, 2023
According to the National Library of Medicine, up to 27% of patients with severe heart valve disorders also suffer from coronary artery disease. Coronary artery disease is a build-up of plaque in the walls of the arteries that supply blood to the heart. Patients with coronary artery disease may experience chest pain, shortness of breath, fatigue and heart attack. It is for this reason that many patients undergo cardiac catheterization (angiogram) prior to heart valve surgery to detect coronary artery disease.
To learn more about the detection and treatment of coronary artery disease, we recently met with Dr. Husam Balkhy, Director of Robotic and Minimally Invasive Cardiac Surgery at the University of Chicago Medicine. Dr. Balkhy is a minimally-invasive specialist who has performed thousands of cardiac procedures and Dr. Balkhy has successfully treated over 50 members of the HeartValveSurgery.com community including Stacy Dubin, Gary Lark and Margaret Caravello.
Key Learnings About Coronary Artery Disease & Heart Valve Disorders
Here are key insights shared by Dr. Balkhy during our interview:
- Coronary artery disease is commonly diagnosed during pre-operative testing for heart valve surgery patients. “Many patients get diagnosed while undergoing the pre-operative workup for their valve therapy,” states Dr. Balkhy. “Say somebody comes in with severe aortic stenosis and they are embarking on having an operation for their aortic valve. They will get a workup which includes a coronary angiogram. Sometimes that coronary angiogram will show that they have a blockage in one or more of the coronary arteries.”
 Cardiac Catheterization (Coronary Angiogram)
Cardiac Catheterization (Coronary Angiogram)
- Cardiac surgeons can perform ‘concomitant procedures’ to treat heart valve disorders and coronary artery disease during the same operation. “Traditionally, that has triggered a combined heart valve and coronary operation. If it’s the aortic valve, that usually entails an aortic valve replacement and coronary bypass. If it’s a mitral valve, it can be a mitral valve repair and/or replacement and a coronary bypass procedure.”
- The University of Chicago Medicine has adopted a heart-team approach to evaluate the best possible treatment for patients. Dr. Balkhy states, “We obviously have adopted the heart team concept. We have meetings at least once a week about all the patients that present for their cardiac care.”
- There are many different treatments that Dr. Balkhy will use for the treatment of coronary artery disease and heart valve disorders including coronary artery bypass grafting (CABG), minimally-invasive robotic-assisted procedures, heart valve reconstruction techniques, non-invasive transcatheter therapies (e.g. TAVR), and combined totally endoscopic coronary artery bypass (TECAB) and TAVR.
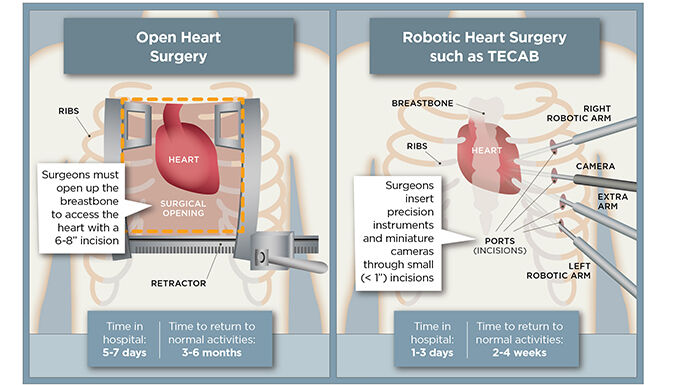 Comparison of Open Heart Surgery to TECAB
Comparison of Open Heart Surgery to TECAB
- To determine the best treatment for each patient, Dr. Balkhy evaluates the patient’s health and risk factors. “We look at the patient, their frailty, obviously their age, their risk factors, and we look at all the things we have to offer in our toolbox and try to do what is best for them,” states Dr. Balkhy.
- Robotic mitral valve repair surgery is a core part of Dr. Balkhy’s practice. “We’re very well-known for our robotic program. The majority of patients that come to my practice are looking for a sternal-sparing operation or procedure,” states Dr. Balkhy. “The patients are coming to me saying okay, I have this and this. Can you still keep my sternum intact? I’m a big believer that keeping the sternum intact is a priority It may not be the highest priority in every patient but it is a priority.”
 Dr. Balkhy Performing Robot-Assisted Mitral Valve Repair
Dr. Balkhy Performing Robot-Assisted Mitral Valve Repair
- The long-term outcomes for heart valve patients with coronary artery disease are favorable. “If we’re doing a TECAB and a TAVR combo, we know the long-term outcomes of a TAVR in the appropriate patients are great. We know the long-term outcomes of a TECAB isolated in our hands – we been doing it for 15 years – are also great. So, there’s no reason why those two things together should not also be great,” states Dr. Balkhy. “Mitral valve repair, we’ve been doing it robotically for 15 years. We know the results of that, and so when we combine that with a PCI to an on-LED target, we know that those outcomes separately are fine. Then when you combine them, they should also be fine.”
Thanks Dr. Balkhy and University of Chicago Medicine!
On behalf of our patient community, many thanks to Dr. Husam Balkhy for sharing his clinical experience and research about coronary artery disease and heart valve disorders! Also, many thanks to University of Chicago Medicine for taking such great care of heart valve patients.
Related links:
- See 50+ Patient Reviews for Dr. Balkhy
- Dr. Husam Balkhy: A Relentless Quest to Make Heart Surgery Less Invasive
Keep on tickin!
Adam
P.S. For the deaf and hard of hearing members of our community, I have provided a written transcript of this interview below.
Video Transcript
Adam Pick: Hi, everybody, it’s Adam with heartvalvesurgery.com, and we are at the American Association for Thoracic Surgery Conference in Los Angeles. I’m thrilled to be joined by Dr. Sam Balkhy, who’s the Director of Robotic Cardiac Surgery at University of Chicago Medicine in Chicago, Illinois. Sam, it is great to see you again.
Dr. Balkhy: Good to see you, Adam. Good to see you.
Adam Pick: Yeah, Sam, I’m hoping you can help expand our education and all the patients in our community specific to not just valvular disease but coronary artery disease. I get lots of questions from patients. They are experiencing both of these at the same time. Can you talk about is this common for patients and if so, what might be considerations in terms of symptoms and risks?
Dr. Balkhy: Yeah, no, great question, Adam, and we get that question a lot from our patients as well. So the majority of patients that present with coronary artery disease usually don’t have an associated or concomitant valvular problem as well, but many do. It’s not an uncommon situation. Many of them get diagnosed while undergoing the preoperative workup for their valve therapy. Say somebody comes in with severe aortic stenosis and they are embarking on having an operation for their aortic valve. They will get a workup which includes a coronary angiogram. Sometimes that coronary angiogram will show that they have a blockage in one or more of the coronary arteries.
Traditionally, that has triggered a combined valve coronary operation, which if it’s the aortic valve, usually entails an aortic valve replacement and coronary bypass. If it’s a mitral valve, it can be a mitral valve repair and/or replacement and a coronary bypass procedure. That’s what the traditional approach has been.
Then there are some patients who come in symptomatic from both conditions, or vice-versa where they come in symptomatic from their coronary disease and it is found at the time of their intraoperative echo that they also happen to have a leaky mitral valve, or an aortic valve that is more than a significant amount of stenosis that has not been diagnosed on its own merit. The conversations about okay, if you’re already in the operating room operating on somebody’s coronaries and they have moderate aortic stenosis, do you replace that aortic valve or not. If they have a moderately leaky valve, do you do something with the valve? There’s a lot of conversation around that.
Adam Pick: For patients who have been told that they may need treatment for both their valve disease and coronary artery disease, how are you treating patients at University of Chicago Medicine?
Dr. Balkhy: That’s a great question. We obviously have adopted the heart team concept, and we have meetings at least once a week about all the patients that present for their cardiac care. We try to customize the therapy not only to the patient but also to the lesion, if you will. When I say lesion, I’m really talking about the site of the blockage of the coronary artery.
If they have a very tight blockage in the main artery, the left anterior descending, which is in a tight situation and it’s not amenable to a stent, those patients can be treated by doing a completely endoscopic robotic operation with a bypass graft to their LED. Now what if they also have an aortic stenosis? Well, are they old enough to be a candidate for a TAVR, and can we do a combined robotic TECAB and TAVR? Or say for example they have a blockage in a less important blood vessel and they have a degenerative mitral valve with a flail P-2 and we know that the best option for that is surgery. In my mind, the best option for that is robotic surgery for the mitral valve.
What we would do in that case is we would also leverage our hybrid concept and treat the mitral valve with the gold standard, which is mitral valve repair and in this case, robotic, and them maybe do a PCI to that obtuse marginal branch number two that is significantly less important than an LED. We look at the patient, their frailty, obviously their age, their risk factors, and we look at all the things we have to offer in our toolbox and try to do what is best for them.
A lot of our patients – as you know, University of Chicago, we’re very well-known for our robotic program, and the majority of patients that come to my practice are looking for a sternal-sparing operation or procedure. We’re look – they’re coming to me saying okay, I have this and this. Can you still keep my sternum intact? I’m a big believer that keeping the sternum intact is a priority It may not be the highest priority in every patient but it is a priority.
Adam Pick: It’s fascinating. You are tailoring care not just for every patient but you’re leveraging all of the resources and assets at the University of Chicago to give the best procedure to that patient at the right time, thinking about their lifetime management of valvular disease and coronary artery disease. I’ve got to ask you. I’m sure patients are wondering, given all these possibilities, what are the outcomes for patients? How do they do after these variable procedures?
Dr. Balkhy: Yeah, no, that’s exactly what we’re doing is exactly what you said and obviously looking at the outcomes is extremely important. I think that we haven’t been doing it long enough to have long-term outcomes, but our – we have long-term outcomes on the isolated procedures separately. For example, if we’re doing a TECAB and a TAVR, the TECAB/TAVR combo, we know the long-term outcomes of a TAVR in the appropriate patients are great. We know the long-term outcomes of a TECAB isolated in our hands – we been doing it for 15 years – are also great, so there’s no reason why those two things together should not also be great.
Mitral valve repair, we’ve been doing it robotically for 12, 15 years. We know the results of that, and so when we combine that with a PCI to an on-LED target, we know that those outcomes separately are fine. Then when you combine them, they should also be fine.
Adam Pick: Wow. Well, Dr. Balkhy, on behalf of all the patients at heartvalvesurgery.com, all the patients all over the world, thanks to your personal efforts and the efforts of your team at University of Chicago Medicine in Chicago, Illinois. Can’t thank you enough for being here today and sharing all these great insights with us.
Dr. Balkhy: Absolutely, thank you very much, Adam, and congratulations on your work. I think you’re doing very important work. Our patients benefit daily from going onto your website, reading about all the stories of the patients they see there, and I always highly recommend it to them.





