Top 6 Mitral Valve Surgery Myths Busted!
Written By: Adam Pick, Patient Advocate, Author & Website Founder
Medical Experts: Michael Acker, MD, Pavan Atluri, MD and Michael Ibrahim, MD, of Penn Medicine
Published: November 16, 2022
Patients diagnosed with mitral valve disease are often confused and misinformed about how to get the best, long-term surgical outcome. To make matters worse, many primary care physicians and cardiologists are not up-to-date about the latest research and technologies used to fix defective mitral valves.
To examine and debunk six common myths about mitral valve surgery, I was very lucky to host a “Surgeon Roundtable” with Dr. Michael Acker, Dr. Pavan Atluri and Dr. Michael Ibrahim from Penn Medicine in Philadelphia, Pennsylvania. During their extraordinary careers, these leading cardiac surgeons have performed over 6,000 heart valve operations.
Key Learnings About Mitral Valve Surgery Myths
In this surgeon roundtable, Dr. Acker, Dr. Atluri and Dr. Ibrahim touch on many great points about mitral valve surgery. Here are the highlights I wrote down following our discussion.
- Myth #1 – Asymptomatic Mitral Valve Disease Patients Do NOT Need An Intervention. Dr. Acker indicates there is significant research and studies that prove asymptomatic patients with mitral regurgitation have better outcomes when a surgical intervention is performed.
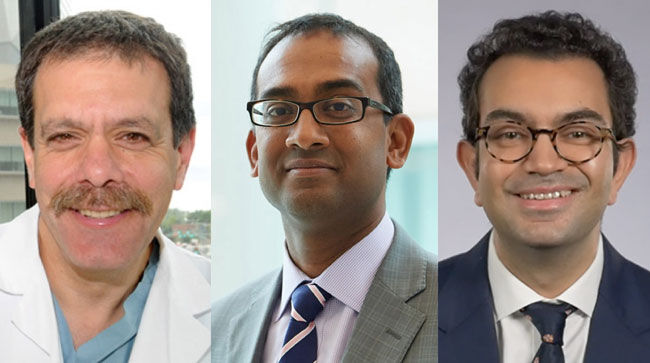 Dr. Michael Acker, Dr. Pavan Atluri, Dr. Michael Ibrahim (Penn Medicine)
Dr. Michael Acker, Dr. Pavan Atluri, Dr. Michael Ibrahim (Penn Medicine)
- Unfortunately, some physicians and cardiologists are not aware of the fact that symptoms are not required (i) for mitral valve disease to cause significant damage to the cardiac muscle and (ii) to warrant an intervention.
- According to Dr. Acker, asymptomatic patients who do not get treatment are at risk for heart failure and decreased survival. Dr. Acker states, “It’s been shown now for about 15 years, after landmark papers, the patients that are completely asymptomatic but have severe mitral insufficiency must have some intervention in order to minimize their chances of going on to heart failure. In fact, in well done, large studies, it’s been shown that patients that are asymptomatic with severe MR that are just followed, their survival is less than patients that have interventions.”
- Mitral valve repair for mitral regurgitation – not mitral valve replacement – is the optimal surgical intervention for patients.
- Myth #2 – Patients With Mitral Valve Disease Who Are Either Elderly Or Sick CANNOT Be Operated On. According to Dr. Acker, this is simply not true. “That is a common held belief among patients, among cardiologists, and among internists, that if the patients are elderly or sick, specifically lung disease, kidney disease, liver disease, frailty, cachectic, that they are too high-risk to undergo mitral valve surgery,” states Dr. Acker. “That’s just simply not true. In centers of excellence that do this all the time and have highly functional teams, we can get the high-risk through these operations, treat their mitral valve disease, and restore them to a quality of life they seek.”
- Myth #3 -Mitral Valve Surgery SHORTENS Patient Life Expectancy. As Dr. Ibrahim suggests this is a common misconception among patients. However, traditional or minimally invasive mitral valve surgery can actually extend a patient’s life. “We are lucky to live in an age where mitral valve surgery can restore normal life survival,” states Dr. Ibrahim. “In good hands, a mitral valve repair should leave you living as long as you would’ve if you had no disease and feeling as well as you can and doing the things that you love doing.”
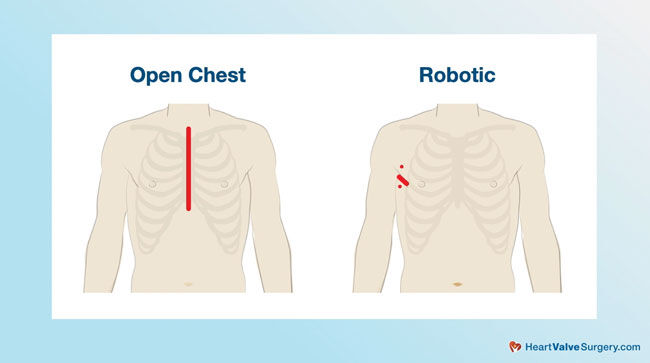
- Myth #4 – Robotic Mitral Valve Repair Surgery Is NOT An Open-Heart Operation. During our interview, Dr. Atluri, who is a robotic mitral valve repair specialist, indicated that robotic mitral valve surgery is an open-heart procedure. Dr. Atluri states, “I can assure you that it is still very much an open-heart operation. In fact, we’re doing the same operation we would do through a traditional sternotomy, through a smaller incision. The patients do benefit from this. They spend less time in the hospital. They recover quicker, get back to life faster.”
- Dr. Atluri suggests there are several questions that patients should ask their potential robotic mitral valve repair surgeon given the complexity of the procedure. Those questions include “How many have they done?”, “How many do they do on an annual basis?”, “What are their outcomes?”, “How often are they able to repair the mitral valve with good long-term durability?”, and “How long does it take them to do it?”
- Myth #5 – Atrial fibrillation (AFib) CANNOT Be Treated During A Robotic Mitral Valve Repair. Dr. Ibrahim refuted this myth and confirmed that AFib can be treated during a robotic mitral valve repair surgery. “I routinely perform atrial fibrillation operations, including the Cox-Maze IV. Especially important to know that we close the left atrial appendage, which is what reduces the stroke risk, and patients are able to return to their normal lives without needing blood thinners in the long-term, through a very small robotic incision.”
- Myth #6 – The MitraClip Is NOT Effective for Low-Risk Patients. Given his direct involvement in the use and research of the MitraClip for mitral regurgitation therapy, Dr. Atluri indicated that physicians currently do not know whether-or-not this is a myth. Dr. Atluri states, “I’m not sure whether that’s a true or false – whether that truly is a myth or not. We won’t know for some time. It might be five-plus years before we have that answer, given that we’re waiting on two key clinical trials which are attempting to address MitraClip versus surgery in lower-risk patients.”
Thanks Dr. Acker, Dr. Atluri, Dr. Ibrahim & Penn Medicine!
Many thanks to Dr. Acker, Dr. Atluri and Dr. Ibrahim for taking time away from their very busy practices to debunk these mitral valve surgery myths! I’d like to thank Penn Medicine for taking care of so many patients in our community including Patricia Garcia, Michael Casey, and Theresa Gusset who had successful heart valve operations at Penn Medicine.
Related Articles:
- The Future of Heart Valve Surgery with Dr. Michael Acker
- Surgeon Q&A: Ross Procedure Reoperations with Dr. Michael Ibrahim
Keep on tickin!
Adam
P.S. For the deaf and hard of hearing members of our community, I have provided a written transcript of this surgeon roundtable below.
Video Transcript:
Adam Pick: Hi, everybody. It’s Adam with heartvalvesurgery.com. This is a very special surgeon round table about six myths of mitral valve surgery. To examine and debunk those myths, I’m thrilled to be joined by three leading cardiac surgeons from Penn Medicine in Philadelphia, Pennsylvania. During their extraordinary careers, Dr. Michael Acker, Dr. Pavan Atluri, and Dr. Michael Ibrahim have performed over 6,000 heart valve procedures. Great to see you, Dr. Acker.
Michael Acker: Always good to see you, Adam.
Adam Pick: Hi, Dr. Atluri.
Pavan Atluri: Hi, Adam.
Adam Pick: Hey there, Dr. Ibrahim.
Michael Ibrahim: Thanks for having us, Adam.
Adam Pick: Thanks so much for joining me on this very important conversation. Dr. Acker, let’s start with a confusing myth for patients, which is asymptomatic mitral valve disease patients do not need an intervention.
Michael Acker: Adam, that is a common misconception by many, not all, but certainly by many, not only patients, but some physicians, even cardiologists. There’s no question that symptoms are the hallmark of mitral valve leak or regurgitation or insufficiency. There is a large group of patients that actually feel pretty well despite having a broken mitral valve and very severe MR.
It’s been shown now for about 15 years, after landmark papers, the patients that are completely asymptomatic but have severe mitral insufficiency must have some intervention in order to minimize their chances of going on to heart failure. In fact, in well done, large studies, it’s been shown that patients that are asymptomatic with severe MR that are just followed, their survival is less than patients that have interventions. Those interventions are basically surgery of different types, but ways of generally repairing the mitral valve, because that’s what is really, in the end, the bottom line you need to do.
Adam Pick: Very helpful, Dr. Acker. Moving on to an often misunderstood Myth Number 2, which is patients with mitral valve disease who are either elderly or sick cannot be operated on.
Michael Acker: That is a common held belief among patients, among cardiologists, and among internists, that if the patients are elderly or sick, specifically lung disease, kidney disease, liver disease, frailty, cathectic, that they are too high-risk to undergo mitral valve surgery. That’s just simply not true. In centers of excellence that do this all the time and have highly functional teams, we can get the high-risk through these operations, treat their mitral valve disease, and restore them to a quality of life they seek.
Adam Pick: Dr. Ibrahim, over to you. A big patient concern in our community is Myth Number 3, which is mitral valve surgery shortens patient life expectancy.
Michael Ibrahim: I hear that a lot, Adam, from patients who obviously have a lot of anxiety when it comes to facing a big operation like a mitral valve repair, whether it be robotic or through a traditional incision. I would flip the statement on its head, that actually mitral valve disease shortens people’s lives and that we are lucky to live in an age where mitral valve surgery can restore normal life survival. In good hands, a mitral valve repair should leave you living as long as you would’ve if you had no disease and feeling as well as you can and doing the things that you love doing. We believe that mitral valve repair can extend survival.
Adam Pick: Dr. Atluri, it is your turn. I get lots of patient questions about Myth Number 4, which is robotic mitral valve repair surgery is not an open-heart operation.
Pavan Atluri: Adam, that is certainly a myth. As someone who does this on a regular basis, as someone who’s done hundreds of these operations, I can assure you that it is still very much an open-heart operation. In fact, we’re doing the same operation we would do through a traditional sternotomy, through a smaller incision, utilizing either the robotic for the robotics or a high-definition 5-millimeter camera if it’s just a straight, minimally invasive approach. The patients do benefit from this. They spend less time in the hospital. They recover quicker, get back to life faster.
From a surgeon standpoint, there is certainly more complexity involved. It’s absolutely critical that you know that your surgeon is well versed in this. What does that mean? How many have they done? How many do they do on an annual basis? What are their outcomes? How often are they able to repair the mitral valve with good long-term durability? How long does it take them to do it? I’ve seen people spend hours trying to repair a valve. I will assure you this is not good for the patient.
We have been very focused on a near 100% repair rate with minimal operative times. Patients as a result have done very well, both short-term, and as we follow our patients for years out, long-term as well.
Adam Pick: Dr. Ibrahim, as you know, many mitral valve patients, up to 35%, struggle with atrial fibrillation, an irregular heartbeat. Myth Number 5 is AFib cannot be treated during a robotic mitral valve repair.
Michael Ibrahim: As somebody who performs a lot of robotic mitral valve operations, I can say that that is not true. I routinely perform atrial fibrillation operations, including the Cox-Maze IV. Especially important to know that we close the left atrial appendage, which is what reduces the stroke risk, and patients are able to return to their normal lives without needing blood thinners in the long-term, through a very small robotic incision.
Adam Pick: Dr. Atluri, the final myth is all about newer technologies for mitral valve therapy. Myth Number 6 is the MitraClip is not effective for low-risk patients.
Pavan Atluri: I’m not sure whether that’s a true or false, Adam, and whether that truly is a myth or not. We won’t know for some time. It might be five-plus years before we have that answer, given that we’re waiting on two key trials which are attempting to address MitraClip versus surgery in lower-risk patients.
I will tell you the data that we have so far will tell you that there’s specific anatomy that is required for a mitral valve to have a successful clip and a good midterm or long-term result. If the right anatomy is not present, we know that the outcomes are suboptimal. Many of those patients go on to then needing surgery to correct the problems, often a very complex surgery.
Adam Pick: With that, on behalf of all patients, I’d like to thank our mitral valve surgery myth-busting team from Penn Medicine.
Michael Acker: Thank you, Adam.
Pavan Atluri: Thanks, Adam.
Michael Ibrahim: Great being with you, Adam.





