Ross Procedure: Which Patients Are Candidates?
Written By: Allison DeMajistre, BSN, RN, CCRN
Medical Expert: Craig Baker, MD, Chief of Cardiac Surgery, Keck School of Medicine of USC, Los Angeles, California
Reviewed By: Adam Pick, Patient Advocate, Author & Website Founder
Published: August 14, 2025
The Ross Procedure is an innovative surgical intervention for patients with severe aortic valve disease. This transformative operation replaces the patient’s diseased aortic valve with his/her own pulmonary valve. Then, a donor valve is implanted in the pulmonary valve position. Many young patients are now finding that it can be an attractive alternative to either a mechanical valve that requires lifelong anticoagulation or a tissue valve that will need to be replaced with a second operation after ten to fifteen years due to valve degeneration.
In the past, critics argued that the Ross Procedure turned a one-valve problem into a two-valve problem. Now, favorable data on patient survivability and valve longevity are creating a strong resurgence in its popularity. However, not every patient is a candidate for the Ross Procedure. Understanding the immediate and long-term consequences of this complex operation can help guide the decision-making process.
To learn which patients are the best candidates for the Ross Procedure, Adam Pick, founder of HeartValveSurgery.com, met with Dr. Craig Baker, the Chief of Cardiac Surgery at the Keck School of Medicine at USC in Los Angeles. Dr. Baker and his colleagues at the Keck School of Medicine have performed over six hundred Ross Procedures and teach other surgeons this complex operation.
Facts About the Ross Procedure and Patient Candidacy
Here are the key insights shared by Dr. Baker:
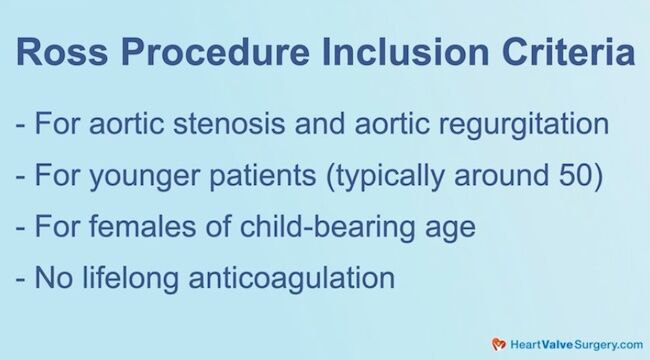
- Younger patients and aortic valve disease. “Patients should know that the Ross Procedure generally treats aortic valve disease,” said Dr. Baker. “That is, typically calcific aortic stenosis, although with the “Inclusion Technique,” it’s also being used for patients with aortic regurgitation. It’s a procedure we typically do in younger patients. There’s really no strict age, but somewhere around 50 years old is a reasonable cutoff, although we’ve done it in older patients. I think because it’s typically done in younger patients, we often see patients with bicuspid aortic valves because they do present at a younger age.” Dr. Baker explained that these younger patients can also include females of childbearing age who don’t want to be on lifelong anticoagulation. He also said that it is a fantastic operation for children who need their aortic valve replaced.
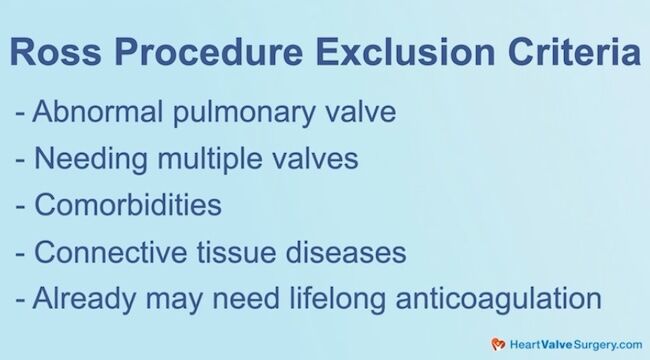
- Patient constraints and those who may not be candidates. “You have to have a normal pulmonary valve,” explained Dr. Baker. “You can’t take out an abnormal valve from the right side of the heart and move it over to the left side and expect that it will do well. We always thoroughly inspect the pulmonary valve, and if there are any concerns about its integrity, we won’t perform the procedure. Also, it is a very complex operation. It’s much different than doing a standard aortic valve replacement with a mechanical or tissue valve. So, it’s probably not for patients who may need multiple valves because they’re already getting another kind of valve.”
- Considerations for a patient’s health history. “It’s probably best not to do in patients with a lot of comorbidities,” said Dr. Baker. “If someone also has coronary disease and doesn’t have the same life expectancy, we probably wouldn’t consider them a candidate. The other group we worry about is patients with connective tissue diseases because we can’t be sure what will happen to that valve.” Dr. Baker explained that patients who are already on lifelong anticoagulation therapy for another reason, like a coagulation disorder, would not be candidates for the Ross Procedure.
- Baker’s number one piece of advice for patients considering the Ross Procedure. “I think the most important thing is that patients get informed,” he said. “They should understand what the Ross Procedure is and whether they are good candidates for it. They also need to understand the complexity of the procedure and find a surgeon and a center that has experience in the Ross Procedure.”
- Baker’s advice for surgeons. “I think for young surgeons out there, you should learn this procedure from somebody who has expertise in it and do your first few with somebody who can help guide you. It is a procedure, not like a standard bypass or valve operation that everyone learns during their training. It takes a special effort to learn this from someone like I did. Dr. Starnes taught me to do it, and then you can learn the right way to do it.”
Thanks Dr. Baker and Keck School of Medicine of USC!
On behalf of all the patients in our community, thank you, Dr. Craig Baker, for everything you and your team are doing at the Keck School of Medicine at USC in Los Angeles, California!
- Discover The Ross Procedure Patient Education Center
- Surgeon Q&A: What Should Patients Know About the Ross Procedure?
Keep on tickin,
Adam
P.S. For the deaf and hard-of-hearing members of our patient community, we have provided a written transcript of our interview with Dr. Baker below.
Video Transcript:
Adam Pick: Hi, everybody. It’s Adam with HeartValveSurgery.com and we are in Los Angeles, California at the Society of Thoracic Surgeons Conference. I am thrilled to be joined by Dr. Craig Baker, who is the Chief of Cardiac Surgery at the Keck School of Medicine at USC in Los Angeles, California.
Dr. Baker, you and I have known each other for a very long time. It is great to see you here at STS.
Dr. Craig Baker: Great to see you, Adam.
Adam Pick: We’re here at STS and a lot of Ross procedure discussion is going on. I know you’re just coming from a wet lab where your team proctored how to do the Ross procedure, and at USC, you guys are now over 600 Ross procedures. So it’s great to have this conversation with you. A big question from the patients is, “ Who are good candidates for the Ross procedure?”
Dr. Craig Baker: Great question, Adam.
I think people, patients should know that the Ross procedure is something that generally treats aortic valve disease. That is typically calcific aortic stenosis, although with the “Inclusion Technique” it’s more often being used for patients with aortic regurgitation.
It’s a procedure that we typically do in younger patients. There’s really no strict age. I think thinking in terms of somewhere around 50 years old is a reasonable cutoff, although we’ve done it in older patients. I think because it’s typically done in patients that are younger, we see patients oftentimes with bicuspid aortic valves, because they do present at a younger age.
I think specifically for young patients, which would include females of childbearing age that don’t want to be on lifelong anticoagulation. It’s a really good operation, and obviously here I’m talking a little bit more on the adult side, but it’s a fantastic operation in children who need the aortic valve replaced.
Adam Pick: Dr. Baker, thanks for sharing that very important information about who the Ross procedure may be for. At the same time, the Ross operation may not be a fit for other patients. Can you talk about maybe some constraints on who the Ross procedure isn’t a good operation for?
Speaker 3: I think if you look at the most obvious constraint, you have to have a normal pulmonary valve. You can’t take out an abnormal valve from the right side of the heart and move it over to the left side and expect it’s going to do good. So, we always very thoroughly inspect the pulmonary valve, and if there’s any concerns about its integrity, we won’t do it.
I think the other thing you have to think about is this is a very complex operation. It’s much different than just doing a standard aortic valve replacement with a mechanical valve or a tissue valve. So it’s probably best not to do in patients that may need multiple valves because they’re already getting another kind of valve already.
It’s probably best not to do in patients with a lot of comorbidities. If someone’s also got coronary disease and maybe doesn’t have the same life expectancy, we probably don’t do it in those patients. I think the other group we worry about is patients with connective tissue diseases because we’re not totally certain what’s going to happen to that valve.
I think the other group you consider out is that patients for whatever reason that may need lifelong anticoagulation for another reason that they’re going to be on it. If they have a coagulation disorder or something like that, then probably gross procedures might not be the best for them.
Adam Pick: Dr. Baker, very helpful learning both the inclusion and exclusion criteria for the Ross procedure. And I’ve got to ask you, for the patients watching this, what is your number one piece of advice for them?
Dr. Craig Baker: I think the most important thing is that patients get informed.
They should really understand what the Ross procedure is. They should understand if they’re good candidates for it. And they should understand the complexity of the procedure. It’s important that patients, when they go to their surgeons, they look for a surgeon and a center that has experience in this procedure.
I think for the young surgeons out there, if anyone’s watching this video, you should learn this procedure from somebody that has expertise in it. and probably do your first few with somebody that can help guide you. It is a procedure, not like a standard bypass operation or a standard valve that everyone learns in the course of their training.
It takes a special effort to learn this from somebody like I did. Dr. Starnes taught me to do this, and then you can learn the right way to do it.
Adam Pick: Wow, well that is extraordinary advice for everybody watching this. And Dr. Baker, on behalf of the patients at HeartValveSurgery.com, patients all over the world, thanks to you and your team at USC for everything you are doing to help Ross procedure patients and all patients with heart valve disease. Thanks for being with me today.
Dr. Craig Baker: Thank you, Adam. My pleasure.



