Modified David Reimplantation Procedure: What Should Patients Know?
Written By: Allison DeMajistre, BSN, RN, CCRN
Medical Expert: Dr. Lars Svensson, Chief, Heart, Vascular & Thoracic Institute, Cleveland Clinic
Reviewed By: Adam Pick, Patient Advocate, Author & Website Founder
Published: July 23, 2024
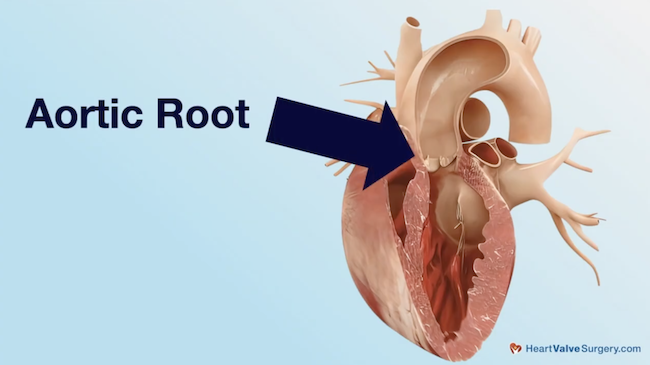
We were privileged to have Dr. Lars Svensson, Chief, Heart, Vascular & Thoracic Institute at Cleveland Clinic, collaborate with us in the following “Surgeon Q&A Interview” about the Modified David Reimplantation Procedure. His surgical experience and extensive research have led to many innovative surgical treatments and techniques, including the Modified David Reimplantation Procedure to replace the aortic root while sparing the aortic valve.
In this video, Dr. Svensson explains the advantages of keeping the native aortic valve rather than replacing it with a mechanical or biological valve and the overall patient outcomes for reimplantation procedures. If you are a patient with an enlarged aortic root and weighing your options for surgery, this comprehensive questions-and-answers session should give you the answers you need for an informed conversation with your surgeon about how to proceed for a successful surgical outcome.
An Introduction to Dr. Svensson
“I’m Lars Svensson. I’m Chairman of the Heart and Thoracic Institute at the Cleveland Clinic, and I’m also the lead surgeon and the Director of the Marfan’s and Connective Tissue Disorders Clinic. Today, we will be talking about the operations done on the aortic root, particularly what we often refer to as the Modified David Reimplantation Operation.”
“It’s important to understand that there are different names for these procedures,” Dr. Svensson said. “There’s valve preserving, where the valve is kept, which can be either done by the remodeling or reimplantation operation.
There’s also what’s called valve-sparing, which is also preservation of the aortic valve leaflets. And again, there’s the reimplantation or the remodeling operation. What we’re going to be talking about is the modification I introduced some 25 years ago, maybe a bit more, for the David Reimplantation Operation.
What is the modification for the David Reimplantation Operation?
“The modification involves putting pledgets on the valve sutures that are used to implant the valve and the freed up aortic valve, what we call the left ventricular outflow tract, into a new plastic tube,” said Dr. Svensson. In addition, the way I started doing it was using what’s called a Hegar’s dilator and tying the sutures down around a Hegar’s dilator that is the correct size for somebody’s body surface area, in other words, size. The importance of that is, firstly, as far as pledgets, I noticed that in some of Tyrone David’s early series, there were sutures that pulled through the mitral valve or other parts of the left ventricular outflow tract and caused fistulas. In other words, openings into different chambers of the heart or damaged surrounding areas. The pledgets make it more secure.”

Dr. Svensson continued, “Secondly, it’s not only the aortic root that increases in size; the annulus, which is where the leaflets are attached, also increases. So the reason for the Hegar’s dilator is to bring it down to a normal size, and I’m convinced that is one of the reasons we have such good long-term results with the reimplantation operation that we modified.”
What are the benefits of keeping the native aortic valve?
“There are a number of benefits to keeping the native valve,” Dr. Svensson said. “Our long-term data shows that the valves hold up very well. The risk of infection is much lower, and the risk of stroke is much lower. In addition, if a young person needs an operation for the aortic root or the aortic valve, they usually get offered a complex operation such as the Ross procedure or a mechanical valve.”
“With a mechanical valve, you have to stay on Coumadin for the rest of your life. A biological valve, if that’s what you choose, is going to fail depending on somebody’s age, anywhere between 5 and 10 years, and then one gets into a sequence of multiple procedures. So, with a reimplantation operation, we know the long-term results are much better.”
What are the patient outcomes?
“One of my trainees, one of the residents, has just analyzed my own data, some 530 patients that I’ve done over the last 20 years, and there were no deaths in that series, and in detail, she analyzed 491 patients that we had long-term follow-up. Ninety-six percent of those patients still had a good functioning valve that had not required a re-operation 15 years after surgery. In other words, if 100 patients had the operation, only four of those patients needed another operation within 15 years of having the modified reimplantation operation.”
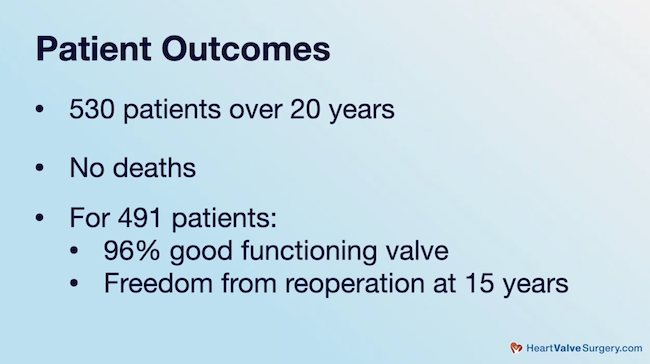
What are the outcomes for patients with connective tissue disorders?
Dr. Svensson told us they did an analysis of 214 patients with connective tissue disorders who underwent a reimplantation and modification procedure. He said, “There were no operative deaths, and the freedom from reoperation at 12 years was 95 percent. So, the reoperation holds up very well long-term.”
Can the Modified David Reimplantation Procedure be used for patients with bicuspid aortic valves, aortic stenosis, and/or aortic regurgitation?
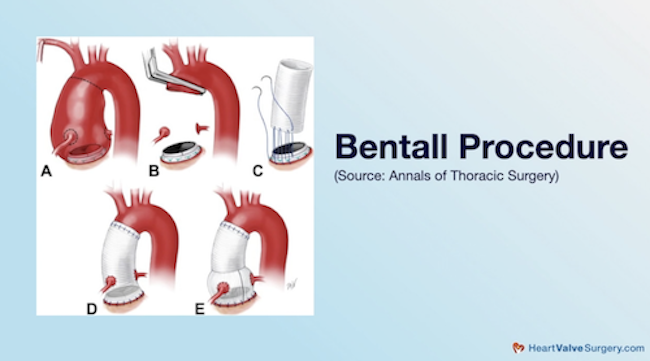
“In patients with bicuspid valves, which is about one to two percent of the population, the ideal operation for somebody who has an enlarged aortic root and a bicuspid valve that’s leaking is really not clearly defined,” said Dr. Svensson. “For patients who have stenosis, calcium buildup on their bicuspid valve, and enlarged root, we go ahead and do a composite valve root replacement, a so-called Bentall operation.”
“In patients with a leaking valve and enlarged root, our data would suggest that the reimplantation operation is probably the best way to go. Our data also suggests that the difference is not significant at this stage between the three leaflet valves and two leaflet valves, the bicuspid valves. They’re holding up pretty well, but we know from other research that bicuspid valves are abnormal and will break down over time.”
“We also do a lot of remodeling operations for bicuspid valves, but I think, on the whole, the reimplantation operation is probably the better way to go for patients with bicuspid valves.”
Is it common for patients with aortic valve disease and an enlarged root to have symptoms?
“There are patients who have symptoms before the operation and those who don’t,” said Dr. Svensson. “The symptoms are related to the aortic valve leaking, so shortness of breath can occur. Chest pain is pretty uncommon, as is dizziness. That’s much more common for a patient who has aortic valve stenosis. In other words, with the narrowing of the valve, patients may have palpitations from the leaking valve or the big left ventricle. Atrial fibrillation can occur, but that’s also uncommon. That’s more related to the mitral valve.”
Is surgery recommended for patients with no symptoms?
“Now, in patients who don’t have symptoms, we look for the size of the left ventricle and if the left ventricle is beginning to deteriorate or the lung functions are beginning to deteriorate. If that’s occurring, then we recommend surgery.”
Can a patient’s height impact when surgery is recommended?
“There’s also the group of patients who have enlarged aortic root, and particularly in the patients who have a family history of aortic dissection that we will operate on before they develop symptoms or signs of a failing heart. So, one of the formulas we use to recommend surgery is we take the cross-sectional area of the aortic root, divide it by the patient’s height in meters, and if that ratio is more than 10, then we recommend surgery.”
“That takes into account the fact that patients who are shorter may, and we’ve shown this, have a higher risk of aortic dissection than somebody who’s tall with an equivalent size aortic root. That comes into the calculation also.”
Are there guidelines that indicate the size at which an aortic aneurysm should be operated on?
“For most patients, when they get up to about five centimeters or so for the aortic root, we recommend surgery. We’ve also shown in patients with bicuspid valves. The enlarged aortic root is a higher predictor of developing aortic root dissection and problems than the ascending aorta size. Now, if somebody has a family history of aortic dissection and, say, Marfan’s or Loeys-Dietz Disorder or any of the other connective tissue disorders, then we often recommend surgery at a smaller size, and that may be at four or five centimeters.”
“There is a group of patients we’ve been looking at who have severe aortic valve regurgitation and not particularly enlarged aortic root. In those patients, we found we can successfully repair the aortic valve in a lot of those patients and do a reimplantation operation for them, even though the root is not very big and the results look pretty good long-term.”
What is the likelihood that the aortic valve can be repaired during a Modified David Reimplantation?
“Now the question sometimes is asked, ‘What is the likelihood that we can repair and keep a valve by the reimplantation and the modifications we use?’ In about a quarter of the patients we will do repairs on the leaflets at the time of the reimplantation to keep the valve. So, for patients who have a three-leaflet valve, I tell them that mostly, 95 percent or better, we can keep the valve for them unless there are big holes in the leaflets. And that’s unusual that they’re so bad that we cannot keep the valves. Occasionally, there are what we call fenestrations. As long as they’re not too big, we can usually keep the valve.”
“The other group are patients with calcium at the annulus where the leaflets are attached to the aorta. We generally do not do a reimplantation operation for those patients.”
Does age impact candidacy for a Modified David Reimplantation Procedure?
“I don’t consider age particularly an exclusion,” said Dr. Svensson. “A couple of weeks ago, I had a patient who was 81 years old. She really wanted to keep her valve, and we did a reimplantation operation for her. She did great. Age is not really a factor, and we’ve done kids. Age is not really a strong factor. Certainly, in elderly patients, we often find calcium, so they may not be a candidate for a modified reimplantation procedure.”
Which tests help Cleveland Clinic determine if the Modified David Reimplantation Procedure is appropriate for a patient?
“As far as whether we can do the operation or not, the echo before surgery is a very good indication, but we can only be sure at the time of surgery, particularly in the patients who have severe leaking valves. Whether that’s due to big holes in the leaflets, or if it’s just from the leaflets being pulled apart by the enlarged annulus or aortic root.”
“The final decision on whether we can keep and repair a valve is related to what we find at the time of surgery.”
How can patients learn more about the Modified David Reimplantation Procedure?
“You’ll see in HeartValveSurgery.com there is a section about the reimplantation operations first described by Tyrone David from Toronto and then also the modification I made many years ago. Most people, I think, are now using modifications of the original operation, and even many of the well-known surgeons who do this operation are now using the modification with the pledgeted sutures and Hegar’s dilators because we think that holds up much better. And it takes away from the complexity of figuring out whether the valve can be preserved or not.”
Thanks Dr. Svensson and the Cleveland Clinic!
On behalf of all the patients at HeartValveSurgery.com, thank you, Dr. Svensson, for sharing your expansive knowledge and insight about the modified David Reimplantation Procedure. Thank you for everything you and your team are doing at the Heart and Thoracic Institute at the Cleveland Clinic!
- Robert Green: A Patient Success Story of Dr. Lars Svensson
- Valve-Sparing Aortic Root Replacement, Including Modified David Reimplantation Surgery
- Valve Reimplantation with Lars Svensson (Video)
Keep on tickin!
Adam
P.S. For the deaf and hard-of-hearing members of our community, I have provided a written transcript this video below.
Video Transcript:
Dr. Lars Svensson: I’m Lars Svensson. I’m chairman of the Heart Thoracic Institute at the Cleveland Clinic and I’m also the lead surgeon and the director for the Marfan’s and Connective Tissue Disorders. Today we are going to be talking about the operations that are done on the aortic root and particularly what we often refer to as the Modified David Re-implantation Operation.
Now it’s important to understand. know that there are different names for these procedures. There’s valve preserving, where the valve is kept, and that can be either by the remodeling or re-implantation operation. There’s also what’s called valve sparing, which is also preservation of the aortic valve leaflets.
There’s the re-implantation or the remodeling operation. What we’re going to be talking about is the modification I introduced some 25 years ago, maybe a bit more, for the David re-implantation operation.
The modification involves putting pledges on the valve sutures that are used to implant the valve and the freed up aortic valve, what we call the left ventricular outflow tract into a new plastic tube. In addition, the way I started doing it was using a, what’s called a Hegar’s dilator, and tying the sutures down around a Hegar’s dilator that is the correct size for somebody’s body surface area, in other words, size.
And the importance of that is, firstly, as far as pledgets, I’d noticed that in some of Tyrone David’s early series, there were Sutures that pull through the mitral valve or other parts of the left ventricular outflow tract and cause fistulas, in other words openings, into other chambers of the heart or damaged surrounding areas.
The pledges make it more secure. Secondly, patients who have these operations, it’s not only the aortic root that increases in size, the annulus, which is where the leaflets are attached, also increases in size. And so the reason for the Hegar’s dilator is to bring it down to a normal size, and I’m convinced that that is one of the reasons we have such good long term results.
With the re-implantation operation that we modified.
There are a number of benefits to keeping the native valve. Our long-term data shows that the valves hold up very well. The risk of infection is much lower and the risk of stroke is much lower. In addition, if a young person needs an operation for the aortic root or the aortic valve, they usually get offered a complex operation such as the Ross procedure or a mechanical valve.
And with a mechanical valve, you then have to stay on Coumadin for the rest of your life. A biological valve, if that’s what you choose, is going to fail depending on somebody’s age, anywhere between 5 and 10 years, and then one gets into a sequence of multiple procedures. So with a reimplantation operation, we know the long term results are much better.
One of my trainees, one of the residents, has just analyzed, my own data, some 530 patients that I’ve done over the last 20 years, and there were no deaths in that series, and in detail, she analyzed 491 patients that we had long term follow up. And 96 percent of those patients still had a good functioning valve that hadn’t required a re-operation at 15 years after surgery.
In other words, the other way to look at this, if 100 patients had the operation, only four of those patients needed another operation within 15 years of having the modified re-implantation operation.
Patients with connected tissue disorders, we did an analysis of that a couple of years ago. 214 patients with re-implantation operations and modification. And there were no operative deaths. And the 12 years was 95%. So, the reoperation really holds up very well long term.
In patients with bicuspid valves, which is about 1 to 2 percent of the population, the ideal operation for somebody who has enlarged aortic root and a bicuspid valve that’s leaking is really not clearly defined. For patients who have stenosis, calcium buildup on their bicuspid valves and enlarged root, those patients we go ahead and do a composite valve root replacement, so called Bentall operation.
In patients with a leaking valve and enlarged root, our data would suggest that the re-implantation operation is probably the best way to go. Our data also suggests that the difference is not at this stage significant between the three leaflet valves and two leaflet valves, the bicuspid valves. They’re holding up pretty well, but we know from other research that bicuspid valves are abnormal and they will, over time, break down.
We do a lot of also remodeling operations for bicuspid valves, but I think on the whole the re-implantation operation is probably the better way to go for patients with bicuspid valves.
For patients who come to us, there are those patients who have symptoms before the operation and those who don’t. The symptoms are related to the aortic valve leaking, and so shortness of breath can occur. Chest pain is pretty uncommon, as is dizziness. That’s much more common for a patient who has aortic valve stenosis.
In other words, narrowing of the valve, patients may have palpitations from the leaking valve or the big left ventricle. Atrial fibrillation can occur, but it’s also uncommon. That’s more related to the mitral valve.
Now, in the patients who don’t have symptoms, in those patients, the things that we look for are the size of the left ventricle, and if the left ventricle is beginning to deteriorate or the lung functions are beginning to deteriorate. If that’s occurring, then we recommend surgery.
There’s also the group of patients who have enlarged aortic root, and particularly in the patients who’ve got a family history of aortic dissection that we will operate before they develop symptoms or signs of a fading heart. So, one of the formulas we use to recommend surgery is we take the cross sectional area of the aortic root, divide it by the patient’s height in meters, and if that ratio is more than 10, then we recommend surgery.
That takes into account the fact that patients who are shorter may, and we’ve shown this, have a higher risk of aortic dissection than somebody who’s tall with equivalent size aortic root. That comes into a calculation also.
For most patients, when they get up to about five centimeters or so for the aortic root, we recommend surgery. We’ve shown in patients with bicuspid valves, the enlarged aortic root is a higher predictor of developing aortic dissection and problems than the ascending aorta size. Now, if somebody has a family history of aortic dissection and, say, Marfan’s Disorder, or Loeys-Dietz Disorder or, any of the other connective tissue disorders, then we often recommend surgery at a smaller size.
And that may be then at 4. 5 centimeters. There is a group of patients that we’ve been looking at who have severe aortic valve regurgitation and not particularly enlarged aortic root. In those patients, we found we can successfully repair the aortic valve in a lot of those patients and do a re-implantation operation for them, even though the root’s not very big and the results look pretty good long term.
Now the question sometimes is asked, “What is the likelihood that we can repair and keep a valve by the re-implantation and the modifications we use?” And we, in about a quarter of the patients will do repairs on the leaflets at the time of the re-implantation to keep the valve. So, for patients who have a three-leaflet valve, I tell them that mostly, 95 percent or better, we can keep the valve for you, unless there are big holes in the leaflets.
And that’s unusual that they’re so bad that we cannot repair the valves. Occasionally, there are what we call fenestrations. As long as they’re not too big, we can usually keep the valve.
The other group of patients are the patients who have calcium at the annulus where the leaflets are attached to the aorta. Those patients we generally do not do a re-implantation operation.
I don’t consider age particularly an exclusion. A couple of weeks ago, I had a patient who was 81 years old. She really wanted to keep her valve and we did a re-implantation operation for her. She did great. Age is not really a factor and we’ve done kids. Age is really not a strong factor.
Certainly in the elderly patients, often we find calcium, and so they may not be a candidate for a modified re-implantation operation.
As far as whether we can do the operation or not, the echo before surgery is a very good indication, but we can only be sure at the time of surgery, particularly in the patients who have severe leaking valves. Whether that’s due to big holes in the leaflets, or if it’s just from the leaflets being pulled apart by the enlarged annulus or aortic root.
The final decision on whether we can keep a valve and repair it is related to what we find at the time of surgery.
You’ll see in HeartValveSurgery.com, there is a section about the re-implantation operations first described by Tyrone David from Toronto and then also the modification that I made many years ago. Most people, I think, now are using modifications of the original operation, and even the many of the well-known surgeons who do this operation now are using the modification with pledgeted sutures and Hegar’s dilators, because we think that holds up much better.
And it takes away the complexity of trying to figure out if the valve can be preserved or not.






