Cardiac Research: The Lifetime Management of Heart Valve Disease
Written By: Allison DeMajistre, BSN, RN, CCRN
Medical Expert: Joseph Zacharias, MD, Cardiac Surgeon, United Kingdom
Reviewed By: Adam Pick, Patient Advocate, Author & Website Founder
Published: November 9, 2025
Over the last 20 years, significant advancements in the diagnosis and treatment of heart valve disease have given many patients their lives back. That said, before patients can take advantage of the best treatments available, they must recognize the symptoms of heart valve disease, receive a diagnosis from their physician, and then be referred to a team of cardiac experts that can create a game plan to repair or replace the diseased valve. When patients follow the correct path to diagnosis and treatment early, their chances of achieving successful outcomes are significantly increased.
To this point, Dr. Joseph Zacharias recently co-authored a new research paper titled, “Lifetime Management of Heart Valve Disease – Treat It Early and Treat It Right the First Time,”. The paper was featured in The Lancet. To learn more, Adam Pick, the founder of HeartValveSurgery.com, recently met with Dr. Zacharias, a leading endoscopic cardiac surgeon in the United Kingdom.
Insights About the Lifetime Management of Heart Valve Disease
Here are the key insights shared by Dr. Zacharias:
- Heart valve disease often goes undiagnosed early on. “I’m going to talk about the publication in The Lancet called ‘Lifetime Management of Heart Valve Disease-Treat It Early and Treat It Right the First Time,” said Dr. Zacharias. “The reason we picked this title is that there is a lot of heart valve disease out there that is not diagnosed. Many patients put a lot of their symptoms of heart valve disease down to just aging, and as part of aging, they presume they are just getting more tired and a little more short of breath.” Dr. Zacharias explained that they’ve found many patients don’t visit their doctors, and even when they do, their symptoms are not thoroughly investigated.

- Educating patients about heart valve disease and promoting early intervention is crucial for achieving positive outcomes. “One of the things we are starting to find is that when a heart valve isn’t treated, the prognosis or lifespan is nearly as bad as some cancers,” said Dr. Zacharias. He explained that they are trying to educate patients by first raising awareness of heart valve disease and second, to have it diagnosed and treated. “Over the last 40 to 50 years, the treatment of heart valve disease has been revolutionized by multiple new and exciting technologies, from transcatheter to endoscopic to robotic. Patients are often frightened about having heart valve surgery because they think it’s through the breastbone, and recovery takes three to six months. However, a lot of these new techniques can have patients home in a few days and back to work in three to four weeks or sometimes even earlier.”
- Early intervention and treatment can cure heart valve disease. Dr. Zacharias said, “We were very fortunate to have a coauthor named Dr. Maurice Enrique Serrano, who was head of cardiology at the Mayo Clinic. One of the things that surprised me was that a significant portion of his work has shown that when patients receive early intervention with the right treatment, heart valve disease can be curative. Your lifespan is just as good as the next person’s. But if you get the patient late and the effects of heart valve disease have affected the heart muscle, then whatever you do, the results are not as good. Sometimes, when they come in really late, their survival is just as bad as cancer.” Dr. Zacharias explained that, given the significant interest in cancer care and treatment, they sought to draw parallels with heart valve disease by highlighting that patients require more comprehensive care networks rather than just isolated points of contact. “We thought the networks would be much wider than just one hospital or one particular health system where people could be sent for the right treatment, even if it meant going somewhere else. In the United States, it may require traveling to a specialist center.”
- Physicians at the specialist center should work as a team. “So, with mitral valve disease, if the valve is regurgitant or leaky, an early intervention is generally curative at any age. But if it’s not, then there are transcatheter options that will also give you a very good result. We are trying to make the point that the care is complementary, and everybody must work as a team.”
- Is it true that even if patients are asymptomatic, the recommendation is that earlier intervention is better? “That is absolutely true,” said Dr. Zacharias. “But there is a caveat to that. The caveat is that you should go to a center of either excellence or a center whose published results are excellent. We believe that the results for asymptomatic patients should be near zero percent mortality and a near 100 percent repair rate. Many surgeons and hospitals achieve that, but cardiologists and networks should be able to identify these centers. Our recommendation would be to travel to a center or a surgeon who has a reputation for providing good results. That is the overall message of our paper.”
- Since you specialize in minimally invasive interventions, would you perform a procedure like mitral valve repair using minimally invasive techniques? “I have a slight problem with the term minimally invasive because it’s a very broad term that covers a lot of conditions and treatments, including transcatheter and half sternotomy or smaller skin incisions. My preferred term is endoscopic. The advantages of endoscopes are that they give both light and magnification. It also helps you learn because you can record your operation. You can re-look at it. So, if you feel you haven’t done a good enough job, you can review it, talk to somebody else, and they can review it, and you can get better.”
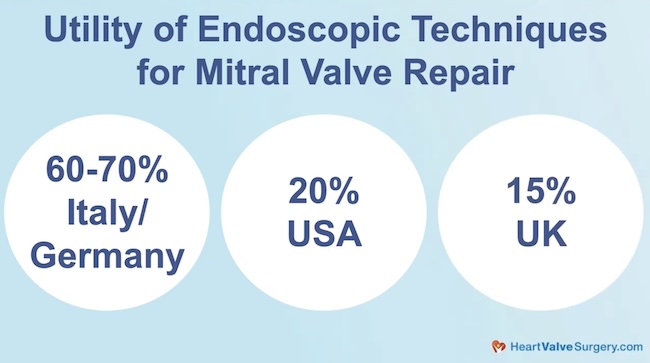
- The goal is to increase the usage of endoscopic techniques. “This meeting is all about endoscopic techniques for cardiac surgery,” said Dr. Zacharias. “Some of them are robotic and some are non-robotic. In Europe, we have been very fortunate to have access to 3D endoscopes for about eight years. In places like Germany or Italy, 60 to 70 percent of mitral valves are repaired using the endoscopic or minimally invasive approach. In the US, it’s about 20 percent. In the UK, at least 15 percent. There is a lot of work to be done, and we hope initiatives like the Endoscopic Cardiac Surgery Club and annual meetings will help both inspire the next generation of surgeons and inform patients and patient groups about its availability. Hopefully, more patients will benefit from what we call a non-sternotomy approach.”
Thanks Dr. Zacharias!
On behalf of all the patients in our community, thank you, Dr. Joseph Zacharias, for everything you and your team are doing to educate patients about the importance of early intervention for the lifelong management of heart valve disease and helping patients return to a normal life expectancy curve.
Related links:
- Heart Valve Experts Unite at Endoscopic Cardiac Surgeons Club Meeting
- Read more from Dr. Zacharias on his Blog
Keep on tickin,
Adam
P.S. For the deaf and hard-of-hearing members of our patient community, we have provided a written transcript of our interview with Dr. Zacharias below.
Video Transcript:
Adam Pick: Hi everybody, it’s Adam with heart Valve surgery.com, and we’re at the Endoscopic Cardiac Surgeon’s Club in Northern Kentucky. I am thrilled to be joined by Dr. Joe Zacharias, who is a leading cardiac surgeon in the United Kingdom. Dr. Zacharias, thanks for being with me today.
Dr. Joseph Zacharias: Thank you for chatting today, Adam. It’s great to be with you.
Adam Pick: We’re here at this meeting, Learning, just a lot of information about minimally invasive techniques At the same time, you recently we’re one of the authors on a publication in The Lancet that I found fascinating.
I was hoping you could help educate our patients in the community about what you found.
Dr. Joseph Zacharias. I’m going to talk about the publication that we got through in Lancet, and it’s called “Lifetime Management of Heart Valve Disease – Treat It Early and Treat It Right The First Time.” The reason we picked this title is because there’s a lot of heart valve disease out there that is not diagnosed.
Many patients put a lot of their symptoms of heart valve disease to just aging. And, as part of aging, they presume they’re just getting a bit more tired, a little bit more short of breath, a little less exercise. What we find is a lot of patients don’t go to their doctors. If they go to their doctors, they’re probably not investigated thoroughly enough.
One of the things we are starting to find is heart valve disease, if not treated, the prognosis or the lifespan is nearly as bad as some cancer. So one of the things that we are trying to educate people is, number one, to think about disease. And number two, once it’s investigated to get it looked at and treated, because over the last 40 to 50 years, the treatment of heart valve disease has just been revolutionized by multiple new, exciting technologies from transcatheter to endoscopic to robotic.
And patients are very frightened of having heart surgery because they may believe that surgery is done through the breast bone and it takes them three to six months to recover. But, a lot of these new techniques can have you back at home in a few days and back to work in three to four weeks or some even earlier.
One of the things that surprised me, and we were very fortunate to have a coauthor called Dr. Maurice Enrique Serrano who was the head of cardiology in Mayo Clinic, was that a lot of his work had shown that if you get patients early and intervene with the right treatment. Heart valve disease can be curative.
The treatments can be curative. Your lifespan is just as good as the next person. But once you get the patient late and the effects of heart valve disease have affected the heart muscle, the pumping chamber, then whatever you do, the results are not as good. And sometimes when they come really late, their survival’s just as bad as cancer.
So, there’s a lot of interest in cancer oncology and we try to draw parallels between heart valve disease and cancer treatment about how maybe we need better networks of care rather than just little points of contact. And we thought the networks would then be much wider than just one hospital or one particular health system where people could be sent for the right treatment, even if it meant going to somewhere else.
Like in the US, it may be traveling to a specialist center. So if you take mitral valve disease, which is one of the things that we focus on, if you have a regurgitant or leaky mitral valve, an early intervention is generally curative at whatever age. But if it is not, then there are transcatheter options as well that will also give you a very good result.
So we were trying to make the point about that and about the fact that it’s all complimentary and everybody has to work in a team.
Adam Pick: For the patients watching this right now, Dr. Zacharias, even if they are asymptomatic, the recommendation is still earlier is better. Is that true?
Dr. Joseph Zacharias: That is absolutely true, but there is a caveat to that.The caveat is that you should go to a center of either excellence or a center that’s published results, which are excellent. So, one of the things that, we feel is the results with patients are asymptomatic should be near 0% mortality and a near a hundred percent repair rate.
Many surgeons achieve it and many hospitals achieve it, but cardiologists and networks should be able to identify these centers and our recommendation would be to travel to a center or a surgeon that produces good results and has a good reputation. And that’s the message of our paper.
Adam Pick: One last point, given your specialty in minimally invasive, and we’re here at the Endovascular Cardiac Surgeons Club for something like mitral valve repair, I’m guessing this is something you do using minimally invasive techniques. Is that correct?
Dr. Joseph Zacharias: I have a slight bug bear with minimally invasive as a term because minimally invasive is a very broad term that covers a lot of, uh, con conditions and treatments and including transcatheter and, you know, half a sternotomy or smaller skin incision. So my preferred, uh, term is endoscopic.
And the advantage of endoscopes are that number one, it gives it light. Number two, it gives magnification. And number three, it helps you learn because you can record your operation. You can re look at it. And so if you feel you haven’t done a good enough job, you can review it, talk to somebody else, they can review it and you can get better.
So this meeting is all about endoscopic techniques for cardiac surgery. Some of them are robotic, some of them are non-robotic. Now we in Europe have been very fortunate to have access to 3D Endoscopes for about eight years. A place like Germany or Italy, 60 to 70% of mitral valves are repaired with the endoscopic or minimally invasive approach.
In the US it’s sort of 20%. In the UK, at least 15%. So there’s a lot of work to be done, and we hope initiatives like the Endoscopic Cardiac Surgery Club and annual meetings help both inspire the next generation of surgeons, but also inform patients and patient groups that this is an. That’s available.
That can be looked into, and I hope more patients will benefit from what, what we call a non-sternotomy approach.
Adam Pick: Dr. Zacharias, on behalf of all the patients in our community, patients all over the world, thanks for everything you and your team are doing to get us back onto that normal life expectancy curve.




