Coronary Artery Disease & Heart Valve Surgery: What Should Patients Know?
Written By: Adam Pick, Patient Advocate & Author
Medical Expert: Dr. Marc Gerdisch, Chief of Cardiac Surgery at Franciscan Health
Published: March 17, 2022
Patients diagnosed with heart valve disease may be surprised to learn that they also suffer from coronary artery disease. And, vice versa, patients diagnosed with coronary artery disease may be confused to learn they unknowingly have valvular disorders including aortic stenosis and/or mitral regurgitation.
Regardless of how or when you are diagnosed with coronary artery disease, it is critical for patients to know that atherosclerosis kills over 360,000 each year in the United States alone, according to the Centers for Disease Control and Prevention.
To learn more about the relationship between heart valve disease and coronary artery disease, we interviewed Dr. Marc Gerdisch, the Chief of Cardiac Surgery at Franciscan Health in Indianapolis, Indiana. A heart valve expert, Dr. Gerdisch has performed over 6,000 cardiac procedures of which more than 4,000 operations involved heart valve repair and/or heart valve replacement therapies.
Key Learnings About Coronary Artery Disease & Heart Valve Surgery
Important learnings shared by Dr. Gerdisch in our interview include:
- There is a distinct and complex relationship between coronary artery disease and heart valve disease.
- Coronary arteries are the blood vessels that feed the heart muscle itself. When the left ventricle squeezes to eject blood into the aorta and out to the body, the first branches that the blood flows into are the branches that go into the heart muscle itself. While the heart is feeding the whole body, it’s also feeding the coronary arteries that feeds the heart muscle.
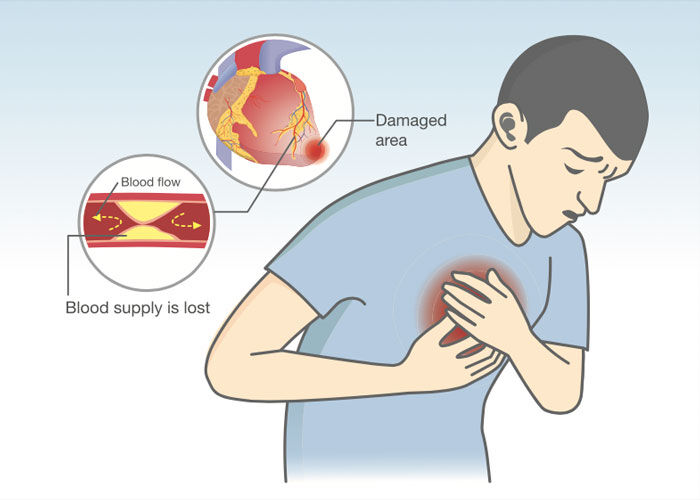
- If the small blood vessels that feed the heart muscle get blocked, the heart is deprived of blood flow and oxygen. Dr. Gerdisch states, “When people say someone had a heart attack, it’s because there was low blood flow or an absence of blood flow to the heart muscle due to blockage of one of those little blood vessels and then that area was deprived of oxygen and then that area can die. Those heart muscles themselves can die. That’s a heart attack.”
- Common symptoms of both cardiac diseases overlap and include chest pain, shortness of breath and fatigue. However, there can be an overwhelming patient symptom of chest pressure prior to a heart attack.
- There is a complex relationship among coronary artery disease and heart valve disease. The process by which aortic valve leaflets become stenotic is similar to the atherosclerotic changes that result from coronary artery disease. Patients who have aortic valve sclerosis have a 50% risk of heart attack (myocardial infarction).
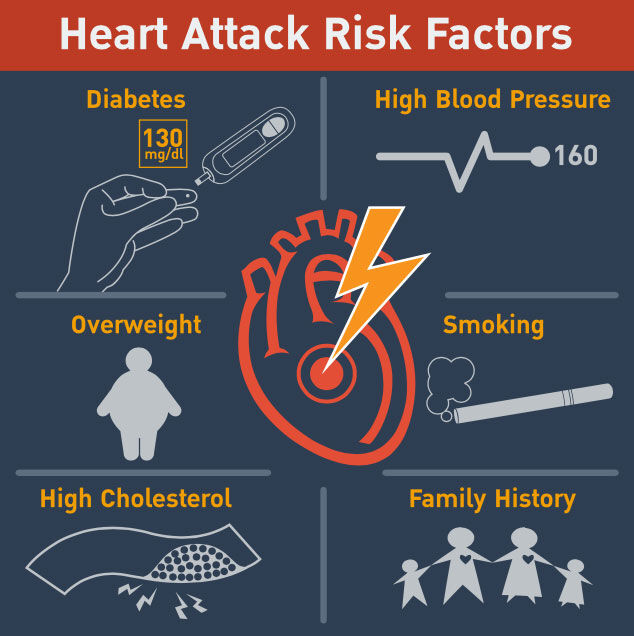
- Managing the progression and the patient risk factors for coronary artery disease (diabetes, cholesterol, weight, smoking) will also help manage the progression of aortic valve disease.
- There are new approaches to heart valve disease therapy that are impacting the treatment of coronary artery disease in patients. Dr. Gerdisch states, “If we’re going to do a transcatheter valve for an elderly patient who has three leaflet valve disease and it’s a straightforward scenario… Then, we do the catheterization and we just happen to find this blocked artery. What do we do with it? Early on, we pretty much treated the coronary artery disease aggressively. Now, the data has come out that often we don’t need to.”
- Heart attacks may cause structural issues within the architecture of the heart that can lead to advanced forms of valvular disorders including mitral valve disease.
- Many patients who have coronary artery disease and heart valve disease may require a “heart team” approach to effectively manage and treat these cardiac disorders with variant therapies that can be open-heart, minimally-invasive and transcatheter. Dr. Gerdisch states, “There’s a relationship there where sometimes we have to address the coronaries when we address the aortic valve. Sometimes we don’t. Or, we put a stent in. Sometimes patients need a transcatheter valve. Sometimes patients need surgery. Then, in the mitral valve, we have this really difficult to manage scenario where there can be injury to the heart muscle, change in the shape of the ventricle impacting the performance of the mitral valve. In those cases, it really requires a team approach and sorting out the best way to treat that patient.”
- Resynchronization therapy using a special type of pacemaker can help patients that struggle with coronary artery disease and mitral valve disease. Dr. Gerdisch states, “When I say resynchronization, I’m talking about a special type of pacemaker that makes sure that both lower chambers of the heart are squeezing synchronously. Interestingly enough, in some of those patients, the mitral valve gets better just by being resynchronized.”
Many Thanks to Dr. Gerdisch & Franciscan Health!!
On behalf of our entire patient community, many thanks to Dr. Gerdisch for sharing his clinical experience and research with our community! Also, many thanks to the Franciscan Health team for taking such great care of heart valve patients.
Related links:
- Heart Surgery Innovations: A New Approach to Pain Management
- Atrial Fibrillation: A Concern for Heart Valve Patients
- Aortic Valve Repair: Top 5 Facts for Patients
Keep on tickin!
Adam
P.S. For the hearing impaired members of our patient community, I have provided a written transcript of this video below.
Video Transcript:
Adam Pick: Hi, everybody. It’s Adam with heartvalvesurgery.com. This is a very important surgeon question and answer session all about coronary artery disease and heart valve surgery. I am thrilled to be joined by Dr. Marc Gerdisch who is the chief of cardiac surgery at Franciscan Health in Indianapolis, Indiana. During his fantastic career, Dr. Gerdisch has performed over 6,000 cardiac procedures of which more than 4,000 involved some form of heart valve repair or heart valve replacement. Dr. Gerdisch, as always, it is great to see you and thanks for being with the heartvalvesurgery.com community today.
Dr. Gerdisch: Thanks, Adam. Always a pleasure. Thanks for having me.
Adam Pick: Yeah, so let’s start with a very important question that I’m sure patients are wondering, which is, what is coronary artery disease?
Dr. Gerdisch: I think that’s a super important question for folks who have heart valve disease, and of course, heart disease in general, because often, it is in tandem. Sometimes things need to be addressed at the same time and it’s related to the coronary artery. Coronary arteries, of course, are of the blood vessels that feed the heart muscle itself. When the left ventricle squeezes to eject blood out into the aorta and out to the body, the first branches that that blood sees are the branches that go into the heart muscle itself. While the heart is feeding the whole body, it’s also feeding itself the blood flow into the coronary arteries that feeds the heart muscle. Sometimes it’s a difficult distinction for people.
These small blood vessels then that feed the heart muscle, if they get blocked completely or partially, they deprive the heart muscle of blood flow and therefore oxygen. When people say someone had a heart attack, it’s because there was low blood flow or an absence of blood flow to the heart muscle due to blockage of one of those little blood vessels and then that area was deprived of oxygen and then that area can die. Those heart muscles themselves can die. That’s a heart attack. Often, these things occur in tandem between valve disease and coronary disease. There’s even some overlap in mechanisms both of the progression of the disease and for how sometimes heart valves are affected by coronary disease.
Adam Pick: Dr. Gerdisch, that’s fascinating. I did not know that. Maybe we can back track. Are there any symptoms that a patient may experience who has coronary artery disease before a heart attack?
Dr. Gerdisch: Yeah, so there are classic symptoms of chest pain or pressure, even shortness of breath which overlaps with valve disease. Again, we might see them in tandem so we have to try to figure out which one is actually causing the symptoms. That can be complicated at times. For example, with a blocked aortic valve and blocked coronary arteries, what’s causing the chest pressure or what’s causing the shortness of breath? The other issue is that, as people develop coronary artery disease, they experience those symptoms differently depending on themselves. For example, folks who have diabetes often won’t have chest pressure. They’ll just develop shortness of breath or they might have an atypical discomfort somewhere in their chest or back, also very true of women. Women tend to have atypical discomfort.
Folks who are at risk for coronary artery disease have to have a little bit of high alert with respect to new onset of symptoms. It might be fairly nuance, some shortness of breath, a little bit of chest pressure, and they don’t put it together. Coronary artery disease and valve disease have some overlap there. Obviously, the very discrete, oh, I’ve got a – I feel like I have an elephant sitting on my chest. That’s classic coronary disease, I’m having a heart attack, but you want to get to it before that. You want to look for those little bit lesser symptoms, less obvious symptoms.
Adam Pick: Dr. Gerdisch, I want to dive a little deeper on the overlap that you’ve been referring to heart valve disease and coronary artery disease. Are these two conditions related? I’m sure the patients are wondering, does one cause the other?
Dr. Gerdisch:That is a topic that we could talk about for a very long time. I’m going to try to summarize it but it’s actually super interesting. The first most obvious relationship is the one that occurs in pathophysiologic and histologic level, which is that coronary artery disease and aortic valve disease, in an otherwise normal tri-leaflet aortic valve, in other words, somebody who is not born with an abnormal aortic valve, they have a relationship. It begins with the fact that the process that occurs in the leaflets of an aortic valve is very similar to the process that happens in the coronary artery, the atherosclerotic changes. So much so that when folks hear that on their echo there was just some aortic valve sclerosis. The aortic valve looks okay but it just has sclerosis. It’s actually a little more important than just a little sclerosis because people who have aortic valve sclerosis have a 50% increase risk of myocardial infraction, a heart attack because that process that is affecting those leaflets and aortic valve is the same as the process that’s affecting their coronary arteries. That’s sclerosis predictive. Furthermore, that sclerosis in the aortic valve, again, just some mild sclerosis, in those patients, at about 1.7% per year, they will progress towards severe aortic valve stenosis.
At the same time, it’s a signal that they have coronary disease. Just seeing some sclerosis in the aortic valve is actually a harbinger. It’s a signal that the patient should be addressing this more globally. How then do they address it? For coronaries, for coronary arteries, it’s statin therapy, so cholesterol lowering medication, addressing diabetes or obesity, stopping smoking. It’s the same kind of process. We all know this. We know that smoking and elevated cholesterol and diabetes all increase the risk of blood vessel disease. The blood vessels can be the blood vessels that feed the heart. At the same time, it will impact progression of the disease in the aortic valve. That’s the first obvious overlap.
Then there are some more subtle ones, for example, someone who has aortic valve stenosis and you happen to find coronary artery disease, but they don’t have any symptoms from the coronary disease, or at least you don’t think so because their heart function is normal. They have a little bit of short of breath. They have a tight lesion in the coronary artery. How do you address that? That depends on the spectrum of the patient’s overall situation. This becomes very complicated and interesting. It’s algorithmic. For example, if someone is – somebody that we’re going to do a transcatheter valve for, elderly patient, three leaflet valve disease, and it’s a straightforward scenario. Then we do the cath and we just happen to find this blocked artery. What do we do with it? Early on we pretty much treated those aggressively. Now the data has come out that often we don’t need to. It depends on how tight the lesion is, what part of the coronary anatomy it is, what the threat is of that lesion.
Another example would be the other end of the spectrum. You’ve got somebody who’s pretty healthy. You’re going to do a minimally evasive aortic valve replacement for them because they have a stenotic aortic valve. The plan is to do this as a parasternal incision. You’re not going to open their sternum. They’re going to have a short hospitalization. Then you do their cath, and lo and behold, you find they have a coronary blockage. Now in many of those cases, those coronary lesions can be addressed just as well with a coronary stent as they can’t with bypass surgery. It doesn’t automatically mean we’ve fled to a full sternotomy. It could be someone who’s best addressed with a stent and then going and having had their minimally evasive valve. Then, though, there are folks who have the combination of fairly extensive coronary disease and valve disease. For the vast majority of those patients, they’re going to be best served with heart surgery where they can get full revascularization of their coronary arteries, bypass surgery. Often using multiple arterial conduits so we can assure they have a good durable operation, and then addressing their valve disease.
There’s another category and that is the patient or patients in whom we find that they have a problem with their valve and it’s due to the coronary arteries. That’s somebody who’s had a heart attack and it’s changed the architecture of the heart and then that affects the mitral valve. You’ll hear about patients with what’s called ischemic mitral valve disease. That’s because the ischemic component means that they didn’t – at some point, they didn’t have adequate blood flow to their heart muscle. That heart muscle was injured. The shape of the heart changed which meant that there was tethering on the mitral valve. Now the mitral valve leaks.
It’s a very – there’s a continuum – a broad spectrum of therapy for these patients as well. When they are surgical and we’re going to do bypass surgery, for example, to treat their coronary artery disease, we want to address their mitral valve, too. In those patients, if we’re going to repair them, often we will not only reshape the valve, the mitral valve, but we’ll put a sling around the papillary muscle, which is the part of the heart that has migrated away from the valve, and we’ll bring that up so that we can reconstruct the normal anatomy between the valve and where the position of the papillary muscle was.
Other times, we’ll have to replace the valve simply because we can’t bring that up enough. If you can imagine, the back of the heart, after it’s been injured, it can balloon out. As it balloons out, it pulls down at the papillary muscles that pulls down on the mitral valve. If we can bring that muscle back up so that the mitral valve is working again, fine. If not, then we might have to replace the valve. Another layer to that is if that balloon has gotten big and scarred, sometimes we’ll cut that scar out, reestablish the shape of the ventricle by repairing what we call an aneurysm of the ventricle, and that in and of itself will restore the geometry of the mitral valve and the papillary muscles.
There’s this relationship between coronary artery disease and aortic valve disease where it’s the same process. There’s a relationship there where sometimes we have to address the coronaries when we address the aortic valve, and sometimes we don’t, or we put a stent in. Sometimes they need a transcatheter valve. Sometimes they need surgery. Then in the mitral valve, we have this really difficult to manage scenario where there can be injury to the heart muscle, change in the shape of the ventricle impacting the performance of the mitral valve. In those cases, it really requires a team approach and sorting out the best way to treat that patient.
I will add one more element to that. Often, patients who have a leaky mitral valve due to coronary artery disease but that coronary artery disease has been treated, by stents or by whatever, sometimes the first line of defense is not an operation or a direct intervention. Medical therapy helps. The other thing is resynchronization therapy. We have to think about layers of intervention and that includes – when I say resynchronization, I’m talking about a special type of pacemaker that makes sure that both lower chambers of the heart are squeezing synchronously. Interestingly enough, in some of those patients, the mitral valve gets better just by being resynchronized. You can see that it’s a team approach. You can see that you need a lot of people having a say and you have to have someone who has a very global view of the pathology.
Adam Pick: Dr. Gerdisch, I am enlightened, to say the least, by that response from you. I did not know about all the complexity, all the different therapeutic approaches for treating valve disease and coronary artery disease. I can’t thank you enough for sharing all the insights that you and your team there at Franciscan Health go through as you plan your surgical missions for your patients. I’ve got to just ask this question as we wrap up here. If you’re a patient and you’ve been diagnosed with coronary artery disease and some form of valve disease, what is your number one piece of advice for patients?
Dr. Gerdisch: Adam, I think you said the word. It’s team. Those of us really deeply involved in these more complex scenarios recognize that we need to work with a team of folks who have a comprehensive understanding of these pathologies. We teach each other. We ensure that each of us is thinking globally about the patient. It really does become not just about the surgeon or cardiologist. It becomes about a lot of other people, too, because these types of disorders typically involve other conditions, diabetes that needs to be managed, other conditions such as hypertension that clearly need to be managed because hypertensive heart disease contributes to changes in heart function and also contributes then to the likelihood of a good outcome for a patient. It’s multidisciplinary approach. It includes obviously surgeons and cardiologists. It includes a team that can address all of these entities in different fashions. Like I said, sometimes it’s surgery with stents. Sometimes it’s surgery and bypass. Sometimes it’s transcatheter valve with or without stenting. All of those options have to be made clear. We really have to be able to present to the patient globally what the options are and also what we would’ve wanted done for ourselves or our loved ones. In order to do that, you have to have a team of people.
Adam Pick: Dr. Gerdisch, I can only tell you how much I appreciate the teamwork mentality that you have cultivated there at Franciscan Health because we have so many patients at the heartvalvesurgery.com community who have come to your facility in Indianapolis there and have had such great surgical results, therapeutic results with your team. On behalf of them and behalf of all the people who are learning from this video, I can’t thank you enough for everything that you’re doing there at Franciscan health in Indianapolis, Indiana.
Dr. Gerdisch: Thank you, Adam. It’s always a pleasure and I really appreciate the ability to be able to communicate some of these educational topics to folks. Thank you so much.






