Bicuspid Aortic Valves: What Should Patients Know About SAVR & TAVR?
Written By: Adam Pick, Patient Advocate, Author & Website Founder
Medical Expert: Christopher Mehta, MD, Cardiac Surgeon, Northwestern Medicine
Published: March 2, 2022
Bicuspid aortic valve disease is one of the most common forms of valvular disorders that impacts 1% to 2% of the general population. As transcatheter aortic valve replacement (TAVR) becomes more prevalent, patients with bicuspid valves often wonder, “Can I get a TAVR?” and “Is a surgical aortic valve replacement (SAVR) better for my two-cusp valve?”
To answer these important patient questions, we interviewed Dr. Christopher Mehta. As you may know, Dr. Mehta is an aortic valve and aneurysm specialist at Northwestern Medicine in Chicago, Illinois.
Key Learnings Bicuspid Aortic Valves, SAVR & TAVR
Here are the key learnings from our discussion with Dr. Mehta.
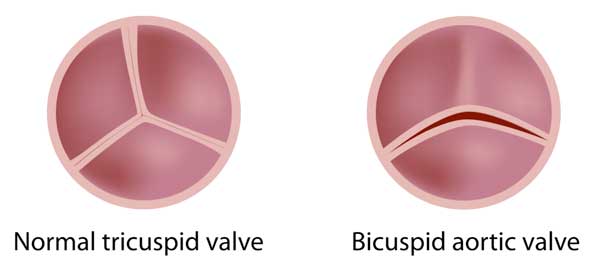
- A bicuspid aortic valve has two cusps instead of a normal aortic valve which has three cusps. Patients with bicuspid aortic valves can be diagnosed with aortic stenosis (a blocked or narrow valve) due to calcification, aortic regurgitation (a leaking valve), or both aortic stenosis and aortic regurgitation.
- Bicuspid aortic valves are commonly associated with aortic aneurysms, an enlarged or dilated aorta, which can put patients at risk for an aortic dissection that can be life-threatening.
- Symptoms of bicuspid aortic valves with aortic stenosis and aortic regurgitation can be chest pain, shortness of breath, light headiness, fainting spells and heart failure. Aortic aneurysms are often asymptomatic. However, patients with severe aortic aneurysms may experience chest pain.
- In 2012, Northwestern Medicine launched the first Bicuspid Aortic Valve Program to research, study, manage and optimize treatment for patients with bicuspid aortic valves. As Dr. Mehta states, “When we identify patients who have bicuspid aortic valves, they are lifelong patients in our program. What that means is that we keep close tabs on them with echocardiograms, CT scan imaging, and MRI imaging to make sure that we really catch when their valve disease or when their aneurysm gets to a point that we need to intervene, either by surgery or noninvasive transcatheter techniques.”
- According to Dr. Mehta, patients with severe aortic stenosis can be treated with surgical aortic valve replacement (SAVR) or transcatheter aortic valve replacement (TAVR). Patients with severe aortic regurgitation are treated using SAVR or aortic valve repair techniques.
- TAVR is a non-invasive procedure that requires no incision to the patient’s chest or ribs, no general anesthesia, and no heart-lung machine. The TAVR stays in place by anchoring itself to the calcium within a stenotic aortic valve.

- Dr. Mehta and the Northwestern Medicine Heart Team use several criteria to evaluate which therapy – SAVR or TAVR – is best suited for a bicuspid aortic valve patient with severe aortic stenosis. Select criteria used by Dr. Mehta and his colleagues include age, morphology (type of bicuspid aortic valve), location of calcification, presence of an aortic aneurysm, and other co-morbidities (e.g. coronary artery disease.)
- According to Dr. Mehta, it is critical that each patient is evaluated for either a SAVR or TAVR. “I would emphasize that no two patients with bicuspid aortic valve disease are the same,” states Dr. Mehta, “Some patients are better suited for surgery. Some patients are better suited for transcatheter aortic valve replacement, or TAVR.”
- SAVR for patients with bicuspid aortic valves has been performed for over 60 years. The use of TAVR for bicuspid aortic valves is a relatively new technology deployed for replacing diseased aortic valves. Dr. Mehta states, “There’s still a lot to learn about who those particular patients are that benefit from TAVR and have a bicuspid aortic valve.”
- Dr. Mehta’s advice for patients with bicuspid aortic valves is (i) to search out a multi-disciplinary, medical team that specializes in SAVR and TAVR and (ii) to seek a second opinion if needed.
Many Thanks Dr. Mehta & Northwestern Medicine
On behalf of our patient community, many thanks to Dr. Christopher Mehta for taking the time to share his clinical experience and research with us. And, many thanks to Northwestern Medicine for taking great care of the HeartValveSurgery.com patients.
Related Links:
- SAVR vs. TAVR: What Should Patients Know (Webinar)
- Emergency Aortic Valve & Aneurysm Surgery
- Which Operation Did Bicuspid Aortic Valve Patient, Jim, Get – TAVR or SAVR?
Keep on tickin!
Adam
Video Transcript:
Adam: Hi, everybody. It’s Adam with heartvalvesurgery.com and this is a special surgeon question and answer session all about the treatment of bicuspid aortic valve disease, including noninvasive transcatheter aortic valve replacement. I am thrilled to be joined by Dr. Christopher Mehta who’s one of the leading cardiac surgeons at Northwestern Medicine in Chicago, Illinois. Dr. Mehta, thanks for being with us today.
Dr. Mehta: Hi, Adam. It’s good to see you again.
Adam: Yeah, so let’s get started, Dr. Mehta. For patients, family members, and friends who might be just learning about bicuspid aortic valve disease, can you explain what is a bicuspid aortic valve?
Dr. Mehta: A bicuspid aortic valve has two cusps, or two leaflets, instead of the usual three. Approximately 1% of the population has a bicuspid aortic valve. There are three heart problems that could potentially be associated with a bicuspid aortic valve. The first is a narrowing of the valve, also known as aortic stenosis, which is caused by accelerated calcification of the valve. That’s typically seen in patients in their 50s and 60s. The second issue is aortic regurgitation, which is leakiness of the valve which causes backward flow of blood into the heart. The third is that bicuspid aortic valves are very commonly associated with aortic aneurysms, which are enlargements or dilations of the aorta. That puts patients at risk for aortic dissection or aortic rupture, two life threatening diseases.
Adam: Dr. Mehta, with 1% of the population potentially having a bicuspid aortic valve, I’m sure patients are wondering, what are the symptoms of this disease and what are its causes?
Dr. Mehta: Bicuspid aortic valve is a congenital condition, meaning you have it since the time you’re born. The symptoms that are associated with aortic stenosis or aortic regurgitation, those two valve problems I discussed, are commonly chest pain, shortness of breath, lightheadedness, fainting spells. In severe situations, both conditions can lead to what’s called heart failure, or inadequate ability of the heart to pump blood forward effectively. Now, aortic aneurysms are commonly asymptomatic, meaning that people don’t really feel symptoms of the aneurysm until it gets really big, and in those cases, sometimes it can cause chest pain.
Adam: Dr. Mehta, given the seriousness of this disease, I understand that Northwestern Medicine has taken a very unique approach to managing and treating bicuspid aortic valves. Can you help us understand that?
Dr. Mehta: When we identify patients who have bicuspid aortic valves, they’re lifelong patients in our program. What that means is that we keep close tabs on them with echocardiograms, CT scan imaging, MRI imaging to make sure that we really catch when their valve disease or their aneurysm gets to a point that we need to intervene, either by surgery or noninvasive transcatheter techniques.
Adam: Dr. Mehta, I want to press pause right here because you brought up the timing of treatment for bicuspid aortic valve. I’m curious to know, and I’m sure the patients are, when is the right time to intervene with treatment?
Dr. Mehta: The right time to intervene is when a patient develops symptoms associated with either aortic stenosis or aortic regurgitation. That’s typically when the aortic stenosis becomes severe or the aortic regurgitation becomes severe or when the aortic aneurysm reaches a size threshold that puts the patient at risk for developing an aortic dissection or rupture. That’s typically between 5 and 5.5 centimeters.
Adam: Dr. Mehta, I’m really curious. Once you and your colleagues determine it’s time for an intervention on a patient with a bicuspid aortic valve, what are the different types of treatment approaches you might use?
Dr. Mehta: Patients with severe symptomatic aortic stenosis that’s associated with the bicuspid valve are treated with two main stays of therapies, either surgical aortic valve replacement or transcatheter aortic valve replacement, or TAVR, which is a novel more minimally invasive way of treating aortic stenosis. Now, patients who develop severe symptomatic aortic regurgitation are treated with surgery, either by aortic replacement, or in some cases, by aortic repair in which we preserve the native leaflets of your own valve and are able to repair to make it a long-term durable option. Patients with aneurysms are treated with surgery as well.
Adam: Dr. Mehta, one of the big questions I have from patients is how does the TAVR stay implanted in the aortic valve position?
Dr. Mehta: The transcatheter aortic valve replacement is performed by snaking a wire through an artery. It’s typically the artery in your groin, the femoral artery. This wire is brought around to the aortic valve. Now, we see this under live x-ray where the wire is going. Then a catheter with the valve is placed over the wire and brought around to the aortic valve. There are two types of TAVR valves. One is a balloon expandable and one is a self-expanding. In both valves are used in the position of the previous aortic valve and essentially pushes the old leaflets out of the way and puts the new valve in there. Once the valve is deployed, it actually anchors to the calcium of the leaflets that are already there and stays in place.
Adam: Dr. Mehta, can you talk about the criteria that you and the Northwestern Medicine team use to evaluate a SAVR versus a TAVR for a bicuspid aortic valve patient?
Dr. Mehta: First thing I would emphasize is that no two patients with bicuspid aortic valve disease are the same. Some patients are better suited for surgery. Some patients are better suited for transcatheter aortic valve replacement, or TAVR. Now, we look at a lot of different criteria in a multidisciplinary heart valve team meeting in order to see which is better for a particular patient. Those criteria include age, the morphology or the type of bicuspid aortic valve a patient has, the location and the degree of calcification that they may have which is causing the aortic stenosis, or any associated aneurysms that may exist. Finally, we look at the patient overall. What are their comorbidities or other medical problems that they have? What are the patient’s social, cultural, and religious preferences? All of that goes together in making our consensus treatment recommendation.
Adam: Dr. Mehta, can you talk about the outcomes that you’re seeing there for patients with bicuspid aortic valve who are having both surgical and transcatheter aortic valve replacement?
Dr. Mehta: One important thing to note is that surgical aortic valve replacement, for patients with tri-leaflet or bicuspid aortic valve, has been performed for over 60 years. We have a lot of long-term data on how durable those valves are. We know that we can perform a surgical aortic valve replacement with low risk in patients with bicuspid aortic valve disease. Now, transcatheter aortic valve replacement as a technology has only been around about a decade. In patients with bicuspid aortic valve disease, we’ve only been using it for even a few years only. There’s still a lot to learn about who those particular patients are that benefit from TAVR and have a bicuspid aortic valve.
Adam: Dr. Mehta, it’s great that you and your team there are looking really closely at the utility of TAVR for bicuspid aortic valve patients. Can you shed some light? Are there any clinical trials happening right now specific to BAV and TAVR?
Dr. Mehta: The major landmark clinical trials that allowed TAVR to be approved for aortic stenosis in low-risk, intermediate-risk, and high-risk patients did not include bicuspid aortic valve patients. That’s a very specific patient population. Now, what we do have is observational data, in other words, real world data of patients with bicuspid aortic stenosis who have received TAVR. We’re still learning a lot about who those particular patients are with the bicuspid aortic valve who may benefit from TAVR.
Adam: Dr. Mehta, I have to ask you. What is your number one piece of advice for a bicuspid aortic valve patient who is considering either a SAVR or a TAVR?
Dr. Mehta: My advice to patients with bicuspid aortic valve disease is to do your homework about heart valve programs. You want to be at a place that offers multidisciplinary care where you’re not only being seen by a cardiologist but also a surgeon and a whole team dedicated to your care. It never hurts to seek a second opinion if you’re unsure. Again, I would emphasize that no two patients with bicuspid aortic valve are alike. Some are better suited with surgery. Some are better suited with transcatheter.
Adam: Dr. Mehta, thanks for providing not just one but several pieces of advice for patients, bicuspid aortic valve patients who are considering either SAVR or TAVR. On that note, I want to thank you so much for taking time away from your very busy practice there are Northwestern Medicine and educating the patients in our community at heartvalvesurgery.com.
Dr. Mehta: Thanks, Adam. I’m happy to help.