Doctor Q&A: Emergency Aortic Valve Disease & Aortic Aneurysm Surgery
Written By: Adam Pick, Patient Advocate, Author & Website Founder
Medical Expert: Christopher Mehta, MD, Cardiac Surgeon, Northwestern Medicine
Published: June 30, 2021
While aortic valve disease is a progressive cardiac disorder that can take years or decades to become severe, patients may require an emergency procedure.
For example, aortic stenosis is commonly referred to as a “silent killer”. Why? According to research by Dr. Eugene Braunwald, once a patient is diagnosed with severe aortic stenosis and that patient experiences symptoms, the survival rate is just 50% after 24 months. That said, a missed aortic stenosis diagnosis could warrant emergency surgery.
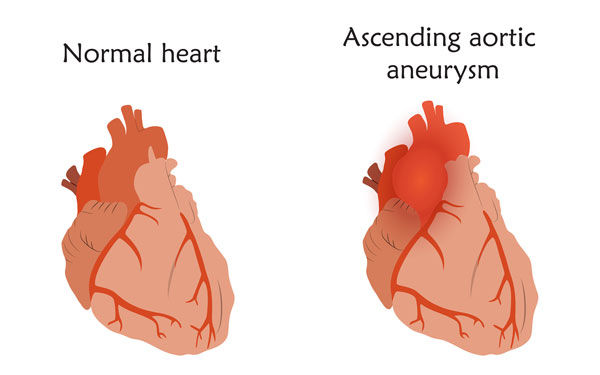
In addition, patients with aortic valve disease often struggle with an aortic aneurysm. The aorta is the largest artery in the body. So, any rupture or dissection of the aorta could be life-threatening. This is another reason that patients may need emergency surgery.
To learn more about emergency operations related to aortic valve disease, we interviewed Dr. Christopher Mehta. As you may know, Dr. Mehta is an aortic valve and aneurysm specialist at Northwestern Medicine in Chicago, Illinois.
Key Learnings About Emergency Aortic Valve & Aneurysm Surgery
Here are the key learnings from our discussion with Dr. Mehta.
- Dr. Mehta knew he wanted to become a cardiac surgeon since he was a child. Dr. Mehta was fascinated by how the heart works and how cardiac surgery can help people feel better. Specific to heart valve therapy, Dr. Mehta believes this is a very exciting time as new, minimally-invasive technologies (e.g. TAVR) are advancing the therapeutic approach to valvular issues.
- Aortic valve disease typically consists of two unique disorders – stenosis (a narrow valve that results from calcium build-up on the valve) and regurgitation (a leaking valve that does not close properly). Both stenosis and regurgitation can causes symptoms including shortness of breath, chest pain, fatigue and dizziness.
 Dr. Christopher Mehta
Dr. Christopher Mehta
- Both aortic stenosis and aortic regurgitation (also known as insufficiency) may cause the heart to enlarge and weaken. Unfortunately, heart failure can result from aortic stenosis and aortic regurgitation as the heart’s ability to “pump blood” is compromised.
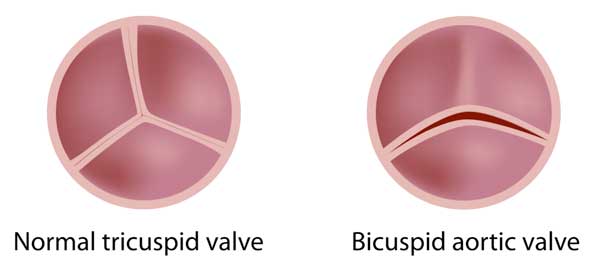
- There is a distinct relationship among the aortic valve and the aorta, which is the largest artery in the body. Abnormal blood flow patterns within an aneurysm can impact the aortic valve and, at the same time, abnormal blood flow pattern across the aortic valve can impact the aorta. Patients with bicuspid aortic valves, a two-cusp valve, are prone to develop aortic aneurysms.
- If an aortic aneurysm progresses, it can cause two potentially life-threatening situations – aortic rupture and aortic dissection.
- Dr. Mehta suggests there is a 1% per hour risk of dying from an aortic dissection within the first 24 hours. Patients with an aortic dissection need to go to the hospital immediately for emergency surgery.
- Risk factors for aortic aneurysms include obesity, smoking and high blood pressure (hypertension).
- Aortic valve disease and aortic aneurysms can be genetic. Dr. Mehta states, “If patients are related to someone who has died of an aortic dissection, these patients should be monitored by their physician for a risk of aneurysm.”
- Common diagnostic tests for aneurysms include CT scans and MRI.
- The goal with monitoring aortic valve disease and aneurysms is to catch them early. Dr. Mehta states, “If we can catch aortic valve disease and if we can catch aneurysms early, we can operate earlier and save lives.”
- There are several different approaches that Dr. Mehta uses to treat aortic valve disease and aneurysms. Those approaches include both minimally-invasive and open-heart procedures that can treat both cardiac conditions during the same procedure.
Many Thanks Dr. Mehta & Northwestern Medicine
On behalf of our patient community, many thanks to Dr. Christopher Mehta for taking the time to share his clinical experience and research with us. And, many thanks to Northwestern Medicine for taking great care of the HeartValveSurgery.com patients.
Related Links:
Video Transcript
Adam: Hi, everybody. It’s Adam with heartvalvesurgery.com, and this is a very important surgeon question and answer session all about emergency cases for aortic valve and aneurysm patients. We’re joined today by Dr. Christopher Mehta, who’s a leading cardiac surgeon at Northwestern Medicine in Chicago, Illinois. Dr. Mehta, are you there?
Dr. Mehta: I’m here. Thanks, Adam.
Adam: Dr. Mehta, thanks so much for joining us today, and we’re going to get to the very important topic about potential life-threatening cases that you deal with at Northwestern Medicine, but before, I’ve got a real quick question about you. When and why did you know that you wanted to become a cardiac surgeon?
Dr. Mehta: I’ve always thought of the heart as a fascinating organ, and even as a young kid, I was in awe of surgeons’ ability to fix heart problems and to make patients feel better, and now, as a practicing cardiac surgeon, it’s very gratifying to have somebody in the operating room, and I can address a heart valve problem or a coronary artery problem or an aorta problem and see almost instant improvement, so that’s very gratifying for me.
Adam: Dr. Mehta, we are so happy you took that path because of all the patients you’re helping out there. Now, let’s talk about valves. Why did you choose valve repairs and valve replacements to become one of your specialties?
Dr. Mehta: This is an exciting time for heart valve treatment and in particular aortic valve treatment. Over the last decade we’ve really seen a lot of innovation in the management of heart valve disease, particularly with the advent of transcatheter aortic valve replacement or TAVR and newer, more minimally invasive open surgical techniques. We as a medical community have shifted to a more heart team approach, a multidisciplinary approach between surgeons and cardiologist where we sit down together and discuss what is the best treatment option for our patients. Between transcatheter and open-heart surgery, we’re really able to address a broad range of aortic valve disease.
Adam: Dr. Mehta, let’s dig deep into one of your specialties, which is the aortic valve. Can you tell the patients out there what is aortic valve disease, and maybe what are some of the symptoms and the risks?
Dr. Mehta: Aortic valve disease falls into pretty much two categories. The first is aortic stenosis, which is a narrowing of the aortic valve, which happens due to hardening and calcium build-up of the valve over time. The second issue is aortic insufficiency, which is also known as aortic regurgitation, in which the aortic valve does not close properly, and blood flow can leak backwards into the heart with each heartbeat. The symptoms of aortic valve disease include chest pain, shortness of breath, fatigue, and lightheadedness. If left untreated, aortic valve disease can lead to more serious problems such as heart failure and even death.
Adam: Specific to how aortic valve disease progresses, can you talk a little bit about that?
Dr. Mehta: As aortic valve stenosis gets worse, the aortic valve gets tighter. A patient’s symptoms will get worse, and the heart has to pump harder in order to get blood flow past that tight aortic valve, and ultimately, the function of the heart can decline. In aortic insufficiency, as that gets worse, there’s more blood volume coming back towards the heart, and in order to compensate for this increased blood volume, the heart actually has to enlarge, and this, too, can lead to heart failure as well.
Adam: Dr. Mehta, the aortic valve is in such a unique part of the heart. Is it often associated with any other forms of cardiac conditions?
Dr. Mehta: The aortic valve can be associated with other cardiac disorders and other conditions. The aortic valve is one of four heart valves that work to pump blood in the appropriate direction. It can also be associated with the heart function or the ability of the heart to adequately pump. The aortic valve can also be associated with aneurysms of the aorta. Now, the aorta is the largest artery in the body, and that comes directly off the heart and supplies blood to the rest of the body.
Adam: Dr. Mehta, there’s a lot of sensitivity for our patient community when we hear about the aortic valve and an aneurysm. Can you really talk about how those two cardiac conditions are related?
Dr. Mehta: That’s a great question, and this is a particular area of interest of mine. Now, aortic valve disease can predispose patients to developing aortic aneurysms, which is a dangerous enlargement of the aorta. This occurs because of abnormal blood flow patterns from a dysfunctional aortic valve. In particular, patients with bicuspid aortic valves, which are valves with two leaflets instead of the usual three – these patients are at risk of early aortic stenosis, commonly found in people in their 50s and 60s, and the development of early aortic aneurysms as well. Now, sometimes the aortic aneurysm comes first and can cause a stretch on the aortic valve causing aortic insufficiency.
Adam: Dr. Mehta, you just referenced potential emergencies related to these cardiac conditions, and I’m real curious to know for all the patients in our community, what types of emergencies can occur?
Dr. Mehta: As an aortic aneurysm progresses, it can lead to two potentially life-threatening situations. The first is aortic rupture, which can be instantly deadly, and the second is an aortic dissection, which causes a tear in the inner lining of the aortic wall leading to a false channel through which blood flows through. Now, this can also be a very deadly situation, and it’s typically a 1% per hour risk of dying from an aortic dissection within the first 24 hours, and so patients with an aortic dissection need to go emergently to the operating room to have emergency surgery.
Adam: Dr. Mehta, I’m guessing one of the really big questions that patients are thinking about right now is what can I do to prevent these life-threatening conditions.
Dr. Mehta: The important risk factors for the progression of an aortic aneurysm and for the development of aortic dissection are obesity, smoking, and high blood pressure, also known as hypertension. These are three risk factors that patients can improve or modify in order to reduce their risk of life-threatening problems. If patients know someone in the family who has died of an aortic dissection or a sudden unknown cause of death or even if they have an aortic aneurysm, then these patients should be monitored by their physician for a risk of aneurysm. If patients know someone in the family who has a bicuspid aortic valve or they know themselves that they have a bicuspid aortic valve or a genetic connective tissue disorder, these patients are also at increased risk of life-threatening problems from aneurysms, and they should be monitored closely by their physician.
Adam: How would you recommend patients monitor these cardiac conditions?
Dr. Mehta: Patients should make sure that they’re following up with their cardiologist and a surgeon, and you can assess heart valves by looking at an echocardiogram either every six months or annually based on what your cardiologist recommends. You can assess the aorta with either a CT scan or an MRI, again, either six months or yearly depending on your physician. If we can catch aortic valve disease, and if we can catch aneurysms early, then we can operate earlier, and we can save lives.
Adam: Saving lives is what you and your team at Northwestern Medicine do there. Maybe could you share with the patients just the treatment process? What types of therapies could you and your team perform to help patients?
Dr. Mehta: For aortic valve disease, we have both surgical options and transcatheter options, and really, it takes a heart team approach with cardiologists and surgeons sitting down together to make an assessment with regards to what is the best treatment option. Now, for aneurysms, especially of the ascending aorta, which comes directly off the heart, these are typically treated with surgery. If you have both an ascending aorta aneurysm and aortic valve disease, those should be treated with open-heart surgery.
Adam: Can these procedures for the both the aortic valve and the aneurysm be performed simultaneously in one procedure?
Dr. Mehta: They can be performed at the same time, so if we’re operating on the aortic valve, we will address the aneurysm at the same time. We always do our due diligence and make sure you don’t have other problems such as coronary artery problems or problems with other valves for example, and so we can address everything at the time of surgery.
Adam: Dr. Mehta, given all the aortic valves and all the aneurysms that you see out there in your patients, I’ve got to ask you this question from our community is what would be your number one piece of advice for patients who’ve been diagnosed with an aortic valve disease and/or an aneurysm?
Dr. Mehta: Make sure you’re following up closely with your cardiologist and your surgeon. We can identify issues with the heart valves using an echocardiogram, and we can identify issues with the aorta with a CT scan or an MRI. Again, if we’re able to catch these things early, and if we can intervene sooner, we can prevent life-threatening issues.
Adam: Dr. Mehta, I can’t thank you enough for taking the time to share this very, very, very important information with the patients in our community. We really appreciate the clinical research that you shared today, and of course, we love the fact that you and your team there at Northwestern Medicine is taking such great care of our patients. Thanks so much, and as we always say here, keep on ticking.
Dr. Mehta: Thanks, Adam. It was great talking with you.




