Pleural Effusion & Heart Surgery: What Should Patients Know?
Written By: Adam Pick, Patient Advocate, Author & Website Founder
Page Last Updated: May 11, 2025
You might have experienced a pleural effusion, or you may know someone who has. Pleural effusions are a common complication after heart surgery. They can be painful and cause concern. You may have questions such as, “What causes a pleural effusion?”, “What are the symptoms?”, and “How is it treated?”
What Are The Pleura?
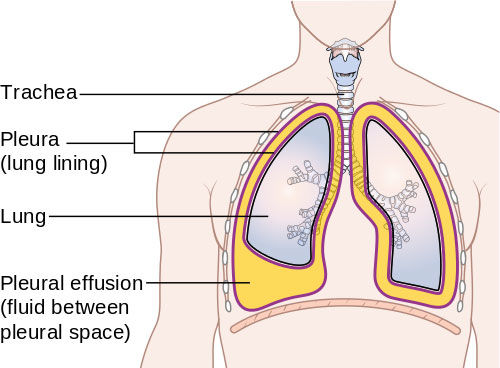
The pleura are two large, thin layers of tissue, or membranes. One lines the inside of the chest cavity (parietal pleurae) and the other wraps around the outside of the lungs (visceral pleura). According to the Cleveland Clinic, the pleura act to lubricate and facilitate breathing. Between these two layers is a small gap called the pleural space that's usually filled with about 3 to 4 teaspoons of fluid.
The Mayo Clinic describes the pleura as “acting like two pieces of smooth satin gliding past each other,” with the pleural fluid serving as a lubricant to allow your lungs to expand and contract when you breathe.
If the pleura becomes inflamed, the layers of the pleural membrane rub against each other like pieces of sandpaper, producing pain when you breathe. The pain only lessens or stops when you hold your breath.
What Is A Pleural Effusion?
As described by the Mayo Clinic, when the pleura becomes inflamed and fluid builds up in the pleural space between the two layers of tissue, it is called pleural effusion (PE). According to the Cleveland Clinic, pleural effusion is sometimes referred to as “water on the lungs”.
The build-up of excess fluid between the layers of the pleura outside the lungs can create pressure, compressing your lung to the point that it partially or completely collapses. This makes breathing difficult and might cause you to cough. The extra fluid can also become infected.
Are Pleural Effusions Common?
According to the American Thoracic Society, pleural effusions are common, with approximately one million cases diagnosed in the U.S. every year. Pleural effusions are a common complication of heart surgery.
According to the European Respiratory Journal, little is known about the cause of many pleural effusions and risk factors for their development remain unclear.
How Often Does Heart Surgery Cause A Pleural Effusion?
Three recent medical studies shed light on this question. A study in the European Respiratory Journal analyzed patients who developed a pleural effusion after a heart surgery. About 40% of the patients developed a pleural effusion, and on average, by day seven post-op. A greater proportion of pleural effusions occurred following a coronary artery bypass graft surgery (CABG) compared to heart valve replacement operations.
A similar study the American College of Chest Physicians analyzed how often patients got a pleural effusion after undergoing CABG, valve replacement, or both. Among the patients in the study, only 6.6% experienced a clinically significant pleural effusion within 30 days following the operation.
Pleural effusions were more frequent in patients with other associated cardiac conditions. Another study in the American Journal of Respiratory and Critical Care Medicine aimed to determine how often a pleural effusion developed related to the type of heart surgery. Pleural effusions in the patients undergoing only CABG surgery, or CABG plus valve surgery was higher than patients undergoing valve surgery only.
In that study, 40% of patients who had a CABG surgery developed a PE in the immediate post-op period. Most of the effusions were small, and they tended to gradually resolve themselves. Occasionally, however, the pleural effusion persisted or a new effusion developed within the first few months after surgery.
What Are The Symptoms Of Pleural Effusions?
According to the Cleveland Clinic, symptoms of pleural effusions include:
- Chest pain
- Dry, nonproductive cough
- Shortness of breath, or difficult, labored breathing
- Orthopnea, which is the inability to breathe easily unless you are sitting up straight or standing
The Cleveland Clinic also notes that some patients with pleural effusion have no symptoms, and only learn of the condition because of a chest x-ray that is performed for another reason.
Should I See My Doctor?
According to the Mayo Clinic, you should call your doctor right away if you experience intense chest pain during breathing. You may need prompt medical care.
To determine if you have a pleural effusion, your doctor might recommend:
- Blood tests, which can tell your doctor if you have an infection or an autoimmune disorder, such as rheumatoid arthritis or lupus.
- Chest X-ray, which can show if your lungs are fully inflating or if there is air or fluid between the lungs and ribs.
- Chest (CT) scan, to show if there is a blood clot in the lung or find other causes of pleuritic pain.
- Ultrasound, which uses high-frequency sound waves to produce precise images of structures within your body.
- Electrocardiogram (ECG or EKG), to help rule out certain heart problems as a cause for your chest pain.
In some cases, your doctor might remove fluid and tissue from the pleural space for lab testing.
How is Pleural Effusion Treated After Heart Surgery?
According to University of Michigan, a minor pleural effusion often goes away on its own without treatment. A pleural effusion can also be treated by removing fluid from the pleural space by using a needle. This may help relieve symptoms, such as shortness of breath and chest pain and help the lungs to expand more fully.
If a pleural effusion is severe, a small catheter tube may be placed in the chest to allow fluid to drain from the space surrounding the lungs. The tube stays in the chest until the fluid is drained or until the doctor removes it.
According to the Cleveland Clinic, pleural effusions that cannot be managed through drainage may require surgery. Your doctor will carefully evaluate you to determine the best treatment option for your pleural effusion and will discuss the possible risks and benefits of each.
Keep Learning!
To help you learn more about pleural effusions, you may also like:
- Patient Q&A: Are Pleural Effusions Common After Heart Surgery?
- Fluid in the Chest (Pleural Effusion) by Healthline
- Pleural Effusion Causes, Signs & Treatment by Cleveland Clinic
References:
MedicineNet
https://www.medicinenet.com/script/main/art.asp?articlekey=4945
Mayo Clinic https://www.mayoclinic.org/diseases-conditions/pleurisy/diagnosis-treatment/drc-20351866
The Cleveland Clinic
https://my.clevelandclinic.org/health/diseases/17373-pleural-effusion-causes-signs--treatment
American Thoracic Society
https://www.thoracic.org/patients/patient-resources/breathing-in-america/resources/chapter-14-pleural-disease.pdf
European Respiratory Journal https://erj.ersjournals.com/content/48/suppl_60/PA2528
American Journal of Respiratory and Critical Care Medicine https://www.atsjournals.org/doi/full/10.1164/rccm.200203-184OC CHEST Journal,
Official publication of the American College of Chest Physicians https://journal.chestnet.org/article/S0012-3692(09)60742-X/fulltext Pleural
Effusion Michigan Medicine, University of Michigan https://www.uofmhealth.org/health-library/abs2938




