Cardiac Research Update: Tissue Heart Valve Replacement Durability for Young Patients
Written By: Andrea Wickstrom, BSN, RN, PHN
Medical Expert: Patrick McCarthy, MD, Executive Director, Bluhm Cardiovascular Institute at Northwestern Medicine
Reviewed By: Adam Pick, Patient Advocate
Published: October 11, 2023
The Centers for Disease Control estimate that 2.5% of the population has heart valve disease. As a result, patients may need a surgical heart valve replacement to prevent debilitating symptoms, health risks and premature death. If the time comes that you need to discuss valve replacement options with a cardiac surgeon, multiple factors will be considered when choosing the best prosthetic device for you. Key considerations may include the patient’s age, projected durability of valve type and quality-of-life.
To learn new research presented at the American Association of Thoracic Surgery Conference (AATS) about tissue heart valve replacements for younger patients, we met with Dr. Patrick McCarthy, the Executive Director of the Bluhm Cardiovascular Institute at Northwestern Medicine in Chicago, Illinois. During his extraordinary career, Dr. McCarthy has performed over 10,000 cardiac procedures including more than 5,000 heart valve operations.
Key Learnings About Tissue Valve Durability
Here are key insights shared by Dr. McCarthy during our interview:
- Dr. McCarthy’s Northwestern Medicine team and a team from the University of Michigan led by Dr. Steven Bolling met to review the data specific to tissue and mechanical valve replacements. Dr. McCarthy and Dr. Bolling debated the dataset during an AATS session called, “How Low Can You Go?”. The goal of the friendly debate was to establish how valve selection – either mechanical or tissue valves – can optimize the lifetime management of valve disease for patients.
- As we have discussed many times here at HeartValveSurgery.com, each patient is unique. Therefore, valve choice (mechanical or tissue) and the right timing for surgery need to be carefully decided by the patient, their surgeon and the entire medical team. Dr. McCarthy states, “What’s most important for the patients to understand is that it’s really their decision. They have to live with that valve for the rest of their life.”
- There are pros and cons to both mechanical and tissue valves.
- Mechanical valves do not typically wear out as fast as tissue valves do, but they have a significant risk of causing stroke due to blood clot formation on the valve. Specific to stroke rate, Dr. McCarthy emphasized, “It’s significant. It’s 3% per year. So, at 10 years… It’s 30%, 20 years 60%.” Patients need to use blood thinners, like Coumadin, for the rest of their life.
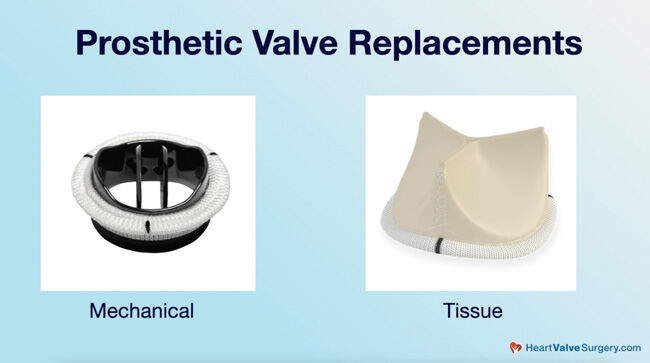
- Tissue valves do not require the patient to use blood thinners. However, tissue valves – which are typically made from cows or pigs – wear out within about 10-15 years. As a result, the patient may need another heart valve surgery in the future.
- The critical questions surrounding tissue valves are “How low can you go (age wise) to safely put a tissue valve in a patient?” and “What can you expect for tissue valve durability?”
- Dr. McCarthy states, “These are really important questions. Previously, the idea was that the valve would wear out faster if the patient is younger. The study presented at the conference showed that durability looked much better than we’ve ever seen before even for patients in the 40-50-60-year age range. It reassured us that for patients with tissue valves who are young in their 50s and 40s, it could still be a good choice for them.”
- Previously, patients who had a tissue valve at a younger age would likely need a second open heart operation in the future when the tissue valve failed. Now, a possibility may be to replace the valve via a transcatheter, non-invasive, valve-in-valve, approach. Instead of re-opening the chest, a catheter can enter the body through the patient’s transfemoral vein (near the groin), be threaded up to the heart, and deploy another valve inside the old worn-out surgical valve. “When you look ahead 20 years, that won’t be the same risk for patients. That’s going to be safer,” Dr. McCarthy added.
- Dr. McCarthy and the Northwestern Medicine team are focused on the lifetime management of heart valve disease for their patients. Dr. McCarthy states, “We absolutely embrace that. We really want to think through with patients and what is going to be the impact to their life to do this.”
Thanks Dr. McCarthy and Northwestern Medicine!
On behalf of our patient community, many thanks to Dr. McCarthy for sharing his new research and insights about tissue valve durability and mechanical valves. Also, many thanks to Northwestern Medicine for taking such great care of heart valve patients.
Related links:
- See Over 175 Patient Reviews of Dr. Patrick McCarthy
- Surgeon Q&A: Stroke Risk Reduction for Heart Valve & Atrial Fibrillation Patients
Keep on tickin!
Adam
P.S. For the deaf and hard of hearing members of our community, I have provided a written transcript of this interview below.
Video Transcript:
Adam Pick: Hey, everybody. It’s Adam with heartvalvesurgery.com and we are at the AATS conference in Los Angeles, California, my home town. I’m thrilled to be joined by Dr. Patrick McCarthy who is the executive director of the Bluhm Cardiovascular Institute at Northwestern Medicine in Chicago. Dr. McCarthy, thanks for being here today.
Dr. McCarthy: Hey, Adam. Good to be with you again.
Adam Pick: Yeah, and so Dr. McCarthy, you are here at the AATS and you’re having a real special presentation. I saw on the program it’s called “How Low Can You Go?” If I remember right, it’s all about tissue valve durability. Can you share with all the patients out there what this conversation is going to be about and the presentation and what are the takeaways for them?
Dr. McCarthy: When we do mitral valve surgery, we frequently try to repair the valve, but sometimes we can’t. Sometimes the valve is just so banged up, especially things like rheumatic fever, maybe an infection, things like that. We have to replace it. Then we have to decide, is it a mechanical valve or is it a tissue valve, like a cow or a pig valve? With Steve Bolling and Matt Romano from the University of Michigan, my Northwestern team and I, we got together and we looked at that data. We presented it and then Steve and I are having a debate. I’m going to win.
Adam Pick: The debate is going to be simply what is right for which patient at which time in their life and how might that relate to the lifetime management of valve disease.
Dr. McCarthy: Correct, so what’s most important for the patients to understand is that it’s really their decision. They have to live with that valve the rest of their life. We as surgeons can put in either a mechanical valve or a tissue valve. It doesn’t matter to us. It’s the same. The advantage to the mechanical valves, theoretically they never wear out, but you run a risk for a stroke. It’s significant. It’s 3% per year, so at 10 years it’s 30%, 20 years 60%. To keep it that low, you have to be on a high dose of coumadin, a blood thinner, not a friendly drug. The tissue valves had been the concern about durability. Will they wear out?
The idea was that, well, they wear out if you’re young faster. How low can you go at that age? Can you put it in a 60-year-old? Is that safe? A 50-year-old or a 40-year-old? What do you expect for durability? These are really important questions. The good news is that the study that we showed is that durability looked much better than we’ve ever seen before for patients even in that 40, 50, 60 age range that patients a year or two before we had thought were young. It reassured us that patients with tissue valve who were young in their 50s, 40s, that could still be a good choice for them. Ultimately, it’s their decision.
Adam Pick: I’ve got to ask. The follow-up question is we’re also hearing about some of these newer transcatheter devices used if a primary tissue valve could fail. Is that something that’s going to tie into your conversation?
Dr. McCarthy: Absolutely, so the discussion that I used to have with my patients would be 20 years ago would be that, okay, some day the valve will wear out. You may need a second operation or open-heart surgery to replace it. If you’re 60 years old, then you might be 80 years old that second time may be pretty formidable. Now there’s a way to replace the valves transcatheter. We can go up through a vein in the leg, across the top, put one inside an old cow or pig valve. When you look ahead 20 years, that won’t be the same risk for patients. That’s going to be safer.
Adam Pick: Dr. McCarthy, the idea of planning for valvular disease throughout the lifetime. Is that something that you do with every patient that you see is what might happen down the road?
Dr. McCarthy: We absolutely embrace that. For patients with aortic valves, mitral valves, valve repair, replacements, we really want to think through with patients what is going to be the impact to their life to do this. They may get a mechanical valve, but every day for the rest of their life, they’re on coumadin. Alternatively, they may get one of those tissue valves and they may have to deal with it again. If they have average luck, it may be 15 to 20 years or even longer. It could be shorter. We plan with them what’s going to happen next so that they know this is going to be what I should be expecting.
Adam Pick: It is great to hear that, great to hear all the incredible things that you and Dr. Bolling are going to be sharing with the community of physicians. Thanks so much for everything that you’ve done for the patients in our community, all the research to stimulate the thinking. It’s amazing what you’ve accomplished throughout your career. I just want to take a moment and thank you for all your help.
Dr. McCarthy: Thank, Adam, and thanks for what you’re doing for the patients as well. It really helps.




