Surgeon Q&A: Treating Mitral Valve Disease in 2020
Written By: Adam Pick, Patient Advocate, Author & Website Founder
Medical Expert: Vaughn Starnes, MD, Keck Medicine of USC
Published: May 4, 2023
During the past 20 years, there has been a rapid transformation specific to the treatment of mitral valve disease. There are new devices, new techniques and new considerations for the management of mitral regurgitation and mitral stenosis.
To answer your questions about the treatment of mitral valve disease, I was very lucky to interview Dr. Vaughn Starnes, the Surgeon-in-Chief of Keck Medicine of USC in Los Angeles, California. As may know, Dr. Vaughn Starnes is heart valve specialist who has successfully treated many patients in our community including Arnold Schwarzenegger, Anna Brusso, Nathan Higginbotham and many others (including me).
Key Points From Dr. Starnes About Mitral Valve Surgery
There were a lot of great points shared by Dr. Starnes during this interview. So, I jotted them down below:
- Dr. Starnes has been treating mitral valve disease for nearly 30 years. Dr. Starnes treats children and adults with heart valve disease.
- According to Dr. Starnes, mitral valve surgery is somewhat like plastic surgery. There is a lot of creativity when performing mitral valve operations.
- While echocardiograms provide Dr. Starnes a great deal of information before surgery, he is always curious to see the actual condition of the mitral valve after he opens the chest.
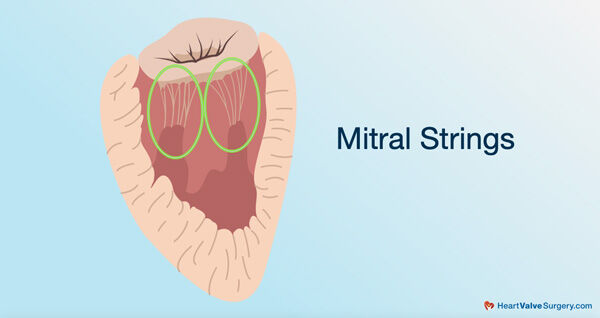
- The mitral valve is a “functional valve” not a “static valve”. The mitral valve does not open and close by pressure differential. The valve is attached to the heart by strings (chords) and papillary muscles.
- In America today… Most disease associated with the mitral valve is called mitral regurgitation, a leaking valve. In the past, mitral stenosis (a narrow valve) was more common due to infection (rheumatic heart disease).
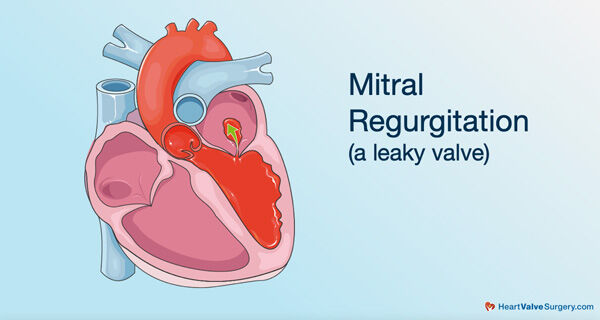
- Symptoms of mitral regurgitation include leg swelling, shortness-of-breath, difficulty exercising and arrhythmias (abnormal heartbeats).
- As mitral regurgitation progresses, the patient is at risk for left ventricular dilation, decreasing left ventricular function leading to heart failure, and a dilation of the atrium which can lead to atrial fibrillation (AFib). AFib, an abnormal heart rhythm, can lead to stroke.
- A mitral valve repair, which may include fixing (or adding) mitral strings and/or implanting a mitral support band (annuloplasty ring), provides advantages for patients including long-term durability and better preserved heart function compared to mitral valve replacement.
- Dr. Starnes performs mitral valve replacement procedures for patients who have mitral valves that are stenotic (narrow) or have a calcified annulus, bileaflet issues and/or coronary artery disease that may cause ischemic mitral disease.
- For younger patients (less than 50 years of age) needing mitral valve replacement, Dr. Starnes may use a mechanical heart valve replacement as it is more durable than a tissue valve which can make the patient susceptible to repeated operations.
- For patients wanting a tissue valve replacement, Dr. Starnes typically uses a pig (porcine) valve in the mitral position. His rational for using a pig valve instead of a cow valve in the mitral position is that Dr. Starnes believes a cow valves may get stiffer quicker and develop a gradient faster in the mitral position. Interestingly, Dr. Starnes typically uses a cow valve in the aortic position.
- New surface coating technologies have been developed to prevent the calcification and the durability of mitral valve replacements.
- The next generation of mitral valve therapy includes the use of transcatheter technologies for mitral valve repair (e.g. MitraClip) and mitral valve replacement. Dr. Starnes believes these technologies have greatly expanded the ability to provide care to high-risk patients.
- While transcatheter devices require no incision to the patient’s chest or ribs, the main advantage for these newer technologies is that patients do not need to be on the heart-lung machine, according to Dr. Starnes. The ability to avoid the use of a heart-lung machine for higher-risk (and elderly) patients, who may have vascular disease, is a huge advantage as it can reduce the potential risk of stroke.
In closing, Dr. Starnes provided excellent advice to patients with mitral valve disease given the different therapeutic options available today.
Understand there is a menu of things that are out there. There’s no one particular one that is best. It’s what’s best for your particular circumstance. If you’re a good surgical risk and you’ve got a mitral valve prolapse or regurgitation, your best option is a surgical repair. If you’re elderly and have got a high-risk for surgery, your best chance is with a MitraClip or even a transcatheter mitral replacement. It’s important that you go to a heart valve center where you have cardiologists and surgeons both looking at your case to give you great advice about what’s best for you.
Thanks Dr. Starnes & USC!!!!
On behalf of our patient, their families and friends, I want to thank Dr. Starnes for sharing his clinical expertise and research specific to the treatment of mitral valve surgery. I also want to thank Dr. Starnes and the entire team at Keck Medicine of USC for providing excellent care to so many patients with heart valve disease!
Related Articles:
Keep on tickin!
Adam
P.S. For the hearing impaired members of our community, I have provided a written transcript of this interview below.
Video Transcript:
Adam Pick: Hi, everybody. It’s Adam with HeartValveSurgery.com. This is a special surgeon question and answer session all about mitral valve surgery. I’m thrilled to share that our guest speaker today is Dr. Vaughn Starnes, who is the Chair of the Department of Surgery and Surgeon and Chief at Keck Medicine of USC in Los Angeles, California.
During his extraordinary career, Dr. Starnes has helped many patients with heart valve disease, including children like Max Page and celebrities who are also governors like Arnold Schwarzenegger. At HeartValveSurgery.com, Dr. Starnes has been an absolute champion. As you probably know, he has many patient success stories. Yes, over 14 years ago, Dr. Starnes performed a double successful heart valve surgery on me. I’d like to bring him into the call. Dr. Starnes, are you there?
Dr. Vaughn Starnes: Thank you so much for that intro. I appreciate all of the compliments that you’re giving me. It’s been my pleasure and will continue to be my pleasure to take care of patients with heart valve disease.
Adam Pick: Dr. Starnes, mitral valve surgery, I understand it is one of your specialties. Can you talk a little bit about why you chose that to be a very important part of your practice?
Dr. Vaughn Starnes: Mitral valve surgery, to me, allows a lot of creativity. Adam, I am also a congenital heart surgeon. Every day, when I’m doing congenital heart surgery, it’s like doing plastic surgery. It’s a little like opening up gifts on Christmas morning; you don’t know exactly what you’re going to get.
Mitral valve surgery is a little like that. You see an echo. You think you know what you’re going to see when you open the chest, but sometimes it’s a little different. It’s the functional valve, it’s not a static valve, that it requires a certain methodology of repairing it to make it functional and gives patients long-term quality of life.
Adam Pick: Yeah, and maybe to help patients who are either newly diagnosed or are going through the treatment selection process, let’s step back and maybe talk about why a patient may actually need their valve fixed. What are the symptoms? What are the causes and potential risks for patients?
Dr. Vaughn Starnes: In America today, most of the mitral valve diseases is actually mitral regurgitation, not mitral stenosis. Years back, the turn of the century when we had strep infections, mitral stenosis from rheumatic heart disease was common, but not so much anymore. Patients today will end up seeing their physician for mitral regurgitation.
The symptoms of that are often leg swelling, shortness of breath, difficulty with mild exercise like climbing maybe a flight of stairs. They may develop arrhythmias. They may develop what they would say fluttering of the heart. These are all signs and symptoms of pretty advanced mitral valve disease.
Adam Pick: When you talk about mitral valve disease, what I have learned over the years is this idea of valve progression or the disease progressing. Can you talk about what a patient may go through as the valve condition gets worse?
Dr. Vaughn Starnes: The biggest problem we have with progressive mitral disease, mitral regurgitation, in particular, is that we get left ventricular dilation, decreasing left ventricular function or heart function leading to heart failure, and a dilation of your atrium. As your atria dilate, you can get into irregular heartbeats, irregular rhythms like atrial fibrillation, atrial fibrillation that’s periodic. That is, you’re in atrial fibrillation one moment, sinus rhythm the next moment, leads you to a risk of stroke because clot formation in the atria.
What you want to do is prevent atrial fibrillation from occurring. Progressive mitral regurgitation or mitral disease leading to that can be a real problem because once you’ve got atrial fibrillation, as anyone would know who has that disease, it’s very difficult to treat. Sometimes multiple meds, blood thinners, ablations, and then maybe finally, surgical ablation with the repair of the valve.
Adam Pick: What exactly is a mitral valve repair? Why might it be advantageous for patients?
Dr. Vaughn Starnes: A mitral valve repair is where we go in and we actually do not replace your valve. That’s the simplest explanation to start with. The mitral valve has got two big leaflets. Usually, it’s the posterior leaflet that’s involved with the disease process. Strangely enough, 80% of that is in the central portion of that leaflet.
Just backtracking a little bit, the mitral valve is a functional valve. It doesn’t open and close by pressure differential. It’s actually attached to the heart with strings and papillary muscles. Sometimes those strings break. The leaflet prolapses like a parachute that has strings cut on it.
When those strings break loose, the valve leaks in that location. We can either go back and resect that portion of the broken strings or we can add new strings in that location. After doing so, we then add a support band to support the entire reparative process.
Now, why would we do that? Number One, we think a repair will last us long or maybe longer than what we have to compare it to, which would be a pig valve or a cow valve. Number Two, we think by having that functional apparatus intact, the strings, the papillary muscles all intact, it preserves the function of the heart better than replacing the valve. Those are the important points I believe in repairing a heart valve.
Adam Pick: Great points about the advantages of mitral valve repair, Dr. Starnes. When might patients need a mitral valve replacement?
Dr. Vaughn Starnes: Mitral valve replacement on echo, you can sit with a patient and say, this valve is not repairable because it could be stenotic, it could have calcium in it, particularly, calcification in the annulus can be a problem for some repairs, you’ve got bileaflet involvement in an elderly patient. More importantly, you may have coronary artery disease is causing what we call ischemic mitral disease. There was a recent study, not so recent anymore, but it showed really that if you tried to repair those ischemic mitrals, a lot of those come back for replacement. If I’ve got a patient that’s 65 years of age or great, has got ischemic mitral, I will often recommend to that patient that a more durable repair is a valve replacement. If I’ve got a lady who’s got a lot of calcium and the annulus sitting out on the leaflets, I’m just going to tell them upfront, the best long-term solution for you is a valve replacement.
Adam Pick: Dr. Starnes, can we talk about the different types of valve replacement devices available to patients who do need a replacement? What can you tell the patients out there about mechanical valves?
Dr. Vaughn Starnes: Yes, a mechanical valve is a valve that’s been around for years. It’s a very durable valve. The only downside is it requires you to be on a blood thinner. In the mitral position, it requires you to be on quite a bit. Whereas in the aortic position, you can take less blood thinner and the valve remains functional.
A lot of people, when they see their cardiologist or their surgeon, and say they’re less than 50 years of age, a mechanical valve is often recommended to them because they’re young. A tissue valve at their age may only last 10 or 12 years, so they’ll be susceptible to repeated operations. A mechanical valve is often the valve that is recommended for a younger person with mitral valve disease.
Adam Pick: Dr. Starnes, I imagine that there is a lot of different types of mechanical valves out there. Is there any one in particular that you’ve used and you’ve seen as a durable device that has helped your patients throughout the years?
Dr. Vaughn Starnes: Adam, there’s basically two mechanical valves out there that are being used. Both of them are bileaflet. One is by Abbott. The other is – blocking on the name of it, but it’s a bileaflet valve.
The valve, of course, I use is the St. Jude Valve. It’s been in the marketplace for over 30 years. It’s a very durable valve. It works well. It’s my valve of choice when I’m putting in a mechanical valve.
Adam Pick: On the flip side of mechanical, Dr. Starnes, I understand there are biological or tissue valves. Can you talk about those options that are available to patients as well?
Dr. Vaughn Starnes: Sure, when you talk about tissue valves, you’re mainly talking about pig valves or porcine valves or bovine or cow valves. Cow valves are mainly made from the heart sac of the cow, pericardium. Of course, the pig valves are pig valves.
Over the years, I’ve been looking at the types of valves in various position. I’ve been at this now almost 30 years. What I’ve seen is that believe it or not, I use a pericardial valve mainly in the aortic position. I use mainly the porcine valve in the mitral position.
My rationale for that is that in the mitral position, the pericardial valves tend to get a little stiffer quicker. They develop a gradient I believe quicker. I have found that the porcine valve functions better in the mitral position than the pericardial valve. I’ve been a mainstay porcine valve user in the mitral position for probably 20 plus years.
Adam Pick: Dr. Starnes, the patients in our community, if there’s one thing I know about them, they love great surgical results. They have a fascination with technology. I have heard that there are some of these new technologies where some of these valves are actually coated with certain types of chemicals to prevent future calcification. Is that something you’re familiar with or have you seen that actually play out during your career as another advantage for certain types of valves?
Dr. Vaughn Starnes: That’s a great point, Adam. I think there are surface coatings now that really have increased the durability, and particularly on the porcine valve. I know every company got its own proprietary way of preventing early calcification. Basically, that is a technology where they hide the aldehyde molecules that prevent – and hopefully prevent calcium from attracting to them. It’s really the glutaraldehyde that we tan the pericardium in or the porcine in that is the radicals that stick out the calcium wants to bind to.
All of these new technologies are really focused on preventing calcium bindings to these molecules on the surface of these valves. That technology has really worked out very well. I do believe it’s increased the durability of these valves.
Adam Pick: Yeah, and in addition to the technology, there is the whole next generation it seems like of valvular therapy, which I know you and your team at USC have been a big part of the research. That is the transcatheter technologies for mitral valve therapy. I’ve heard a lot about mitral valve repair using devices like the MitraClip. How has that helped your patients there at USC?
Dr. Vaughn Starnes: There’s a lot of transcatheter technologies you’ve introduced. There’s actually valve replacement technology now with catheter-based technology. What that has really done is it’s allowed us to expand care to patients that would otherwise be high risk for surgery.
Sick patients got a 20 or 30% risk for a complication or even death with surgery with mitral valve disease. We can offer MitraClip or even a transcatheter valve if the clip is not appropriate to these patients. We’ve expanded the ability to offer an intervention for their mitral disease that might not involve the rigors of surgery, opening their chest, and obviously, the post-operative recovery.
Adam Pick: Yeah, maybe to contextualize for the patients listening, you talk about the rigors of surgery versus transcatheter and the fact that these patients who are at high-risk, they do not need to have their sternum – no incision to the sternum, I think no insertion to the ribs. Are there any other advantages that patients might want to know about a transcatheter approach and what their recoveries might be like compared to surgical?
Dr. Vaughn Starnes: Yeah, with a transcatheter approach, I think the biggest advantage is they don’t have to be on the heart-lung machine. The incision is an issue, not the biggest issue as I think the risk of an elderly patient, particularly with vascular disease, going on a heart-lung machine with the attendant risk of stroke. It’s just one of the things that we do with surgery that we need; it’s a device we can’t get around.
If we can avoid that in an elderly patient that may already have some complications, high surgical risk, that’s the biggest thing that we get around with our transcatheter therapies. That’s huge. A patient that gets a transcatheter clip, a MitraClip, actually can go home the next day. It’s remarkable how we can offer some benefit without giving the long, post-operative recovery that would be necessitated by someone that may have surgery for that same process.
Understand for patients, there is if you would, a menu of things that are out there. There’s no one particular one that is best. It’s what’s best for your particular circumstance.
If you’re a good surgical risk and you’ve got a mitral valve prolapse or regurgitation, your best option is a surgical repair. If you’re elderly and have got a high-risk for surgery, your best chance is with a MitraClip or even a transcatheter mitral replacement. It’s important that you go to I think a heart valve center where you have cardiologists and surgeons both looking at your case and to give you great advice about what’s best for you. I think also, Adam, you’re doing a great service to the general population by putting the information out there that they know what they could select from and how to choose from it.
Adam Pick: Thanks so much for the kind words, Dr. Starnes. I’ve got to thank you even more for that advice because I’ve got to tell you, the last question I was going to ask you is what your Number One piece of advice, but I think you just shared about five or six great pieces of advice. I want to thank you so much for really distinctly helping the patients understand what their mindset may want to go through as they get ready for a very significant procedure in their life.
With that, I guess we can wrap this up. Thanks so much for your time, Dr. Starnes. Thanks so much for all the great things you’re doing there at USC. Again, I just can’t thank you enough for everything that you and your team is doing. Thank you.
Dr. Vaughn Starnes: Adam, it’s been wonderful to be with you. Thank you very much.





