Surgeon Q&A: Treating Bicuspid Aortic Valves & Aortic Aneurysms
Written By: Adam Pick, Patient Advocate, Author & Website Founder
Medical Expert: William Brinkman, MD, Director of the Thoracic Aortic Clinic at Baylor, Scott & White The Heart Hospital – Plano
Published: October 2, 2020
Bicuspid aortic valves are the most common form of congenital heart disease. According to reports, between 1% to 2% of the general population have a bicuspid aortic valve.
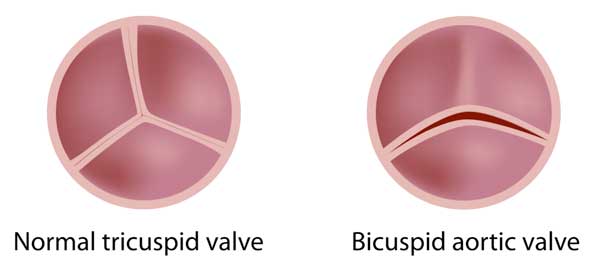
While normal aortic valves have three heart valve leaflets. A bicuspid aortic valve has just two leaflets. During pregnancy, two of the aortic valve leaflets fuse together. Over time, a bicuspid aortic valve may cause aortic stenosis and/or aortic regurgitation. In addition, bicuspid aortic valves are associated with aortic aneurysms, a dangerous form of heart disease that can unexpectedly rupture the aorta. The aorta is the main artery that carries blood from your heart to the rest of your body.
To answer your questions about bicuspid aortic valves, aortic aneurysms and different treatment options, I interviewed Dr. William Brinkman, a leading heart surgeon and the Director of the Thoracic Aortic Clinic at Baylor, Scott & White The Heart Hospital – Plano. As many of you know, Dr. Brinkman has successfully treated many patients in our community including John Martin, Mark Mobley and Randy Neal.
Key Facts About Bicuspid Aortic Valve Treatment
Dr. Brinkman shared several great points about bicuspid aortic valve treatment. Here are some of the highlights I jotted down:
- Bicuspid aortic valves are genetic although a single a single gene is not responsible for the defect, it is multi-factorial.
- Patients with bicuspid aortic valves can be asymptomatic, without symptoms, while other patients may experience shortness of breath, fatigue, chest pain and abnormal heart rhythms.
- Bicuspid aortic valves can impact people differently at various stages of life – from children to the elderly.
- This cardiac condition can be fatal – especially when it causes aortic stenosis.
- Bicuspid aortic valves are related to aortic aneurysm given their embryology. There is debate as to whether a BAV causes an aneurysm or whether an aneurysm causes a BAV. Risks associated with aortic aneurysms include dissection and, unfortunately, death. John Ritter, the comedian, had a bicuspid aortic valve and an aortic aneurysm that dissected which took his life.
- Dr. Brinkman uses several different options to treat bicuspid aortic valves depending on the underlying disorder (e.g. aortic stenosis, aortic regurgitation and the presence of an aneurysm). Common treatment options that Dr. Brinkman use including aortic valve replacement, aortic valve repair, the David Procedure, the Ross Procedure and transcatheter aortic valve replacement for re-operations.
- If an aortic valve is leaking, Dr. Brinkman can perform an aortic valve repair.
- A tight “coaptation” of leaflets is the goal of heart valve repairs which can result in long-term durability for patients without re-operation.
- Dr. Brinkman and his team, including Dr. William Ryan, have performed nearly 300 Ross Procedures for bicuspid aortic valve patients that (i) do not want to be on Coumadin, (ii) are younger, (iii) have an active lifestyle and (iv) may have the opportunity for a transcatheter valve replacement if the aortic or pulmonary valve fails in the future.
- To treat aneurysms of the ascending aorta, Dr. Brinkman is primarily interested in the size of the aneurysm and the current condition of the aortic valve. After that assessment is complete, Dr. Brinkman may complete a Bentall Procedure, a Ross Procedure, or a valve-sparing procedure. If possible, Dr. Brinkman always tries to preserve the patient’s tissue when treating bicuspid aortic valves if patient has an aneurysm.
- Transcatheter aortic valve replacement (TAVR) can be used for more complex procedures including a Bentall procedure, a Ross Procedure, or a David Procedure. The size of the valve is an important consideration when considering a TAVR “Valve-in-Valve” re-operation.
- Dr. Brinkman’s advice to patients is to find a specialist in bicuspid aortic valve and aneurysms. It’s important to identify a cardiologist or surgeon who is very knowledgable about the guidelines for treating these conditions.
Thanks Dr. Brinkman!!!
On behalf of our entire community, thanks so much to Dr. Brinkman for sharing his clinical experience and research with our community. I would also like to thank the entire team at Baylor, Scott & White The Heart Hospital – Plano for their support and care of the patients in our community.
Keep on tickin!
Adam
P.S. For the hearing impaired members of our community, I have provided a written transcript of this video interview below.
Video Transcript
Adam Pick: Hi, everybody, it’s Adam with HeartValveSurgery.com, and today we have a special question-and-answer session with Dr. Bill Brinkman, should say Dr. William Brinkman. I’m going to bring him in. Dr. Brinkman, are you there?

Dr. Brinkman: Yeah, hello. Hey, Adam.
Adam Pick: Hey, great to have you with us today, Dr. Brinkman. I want to start – we’ve got a great topic, and it’s very near and dear to my heart because I had a bicuspid aortic valve, and that’s what we’re going to be talking about today, which is one of your specialties, correct?
Dr. Brinkman: Yes, sir, yep.
Adam Pick: Before we get to it, Dr. Brinkman, maybe we can start. You do so many neat things in your practice. Can you share a little bit about how long you’ve been in practice and your specialties there at Baylor Scott & White Health in Plano, Texas.
Dr. Brinkman: Sure. Well, I’ve been in practice since 2007, and I’ve been focused on diseases of the thoracic aorta, the aortic root, and the aortic valve. I’m a cardiac surgeon there in north Texas, but I’m also the director of our thoracic aortic clinic, so aneurysms, leaky aortic valves, bicuspid valves. That’s the kind of stuff I love to deal with and help people with.
Adam Pick: Yeah, and Dr. Brinkman, for the folks in our community who many not know you, they really should know you’re no stranger to HeartValveSurgery.com. You’ve helped so many patients here learn about – get educated, get empowered, an ultimately get treatment. Thanks for all the work you’ve done in the past. Now let’s talk about bicuspid aortic valves. Can you maybe start by helping the patients out there understand what is a bicuspid aortic valve? What are the symptoms and potentially the causes and unfortunately, the risks?
Dr. Brinkman: Well, bicuspid aortic valve is an aortic valve that has – two of the leaflets are fused, and normally you have three leaflets. Many times, those valve work fine but sometimes, it causes either the valve to leak or the valve not to open well and if that’s the case, the person with the problem can have some symptoms, and that’s where we step in. It’s actually the most common congenital heart defect there is, so it’s quite common actually.
Adam Pick: Dr. Brinkman, I’m sure there are some folks out there listening who maybe they know a relative who has had a bicuspid aortic valve. Can you share about are there any genetic components to this form of cardiac disease?
Dr. Brinkman: Yes, there are genetics associated with it. It does tend to run in families, but it’s not as simple as one gene. It’s multi-factorial, but we’re learning more and more about the genetics of it as time goes on.
Adam Pick: In terms of the impact on patient health, what might a patient who has a bicuspid aortic valve experience? Can you talk about the symptoms in our patients? Always – are they always symptomatic?
Dr. Brinkman: They’re not always symptomatic. Many are asymptomatic, and it’s really a spectrum of disease. You may have even little children who are born with a severe valve dysfunction from a bicuspid valve, and they may need to have surgery young, or you may have someone who lives their whole life and dies of other causes in their 80s or 90s, and they happen to have a bicuspid valve. It’s something that is associated with valve dysfunction but not necessarily causing problems.
Adam Pick: Can you maybe share if somebody was to be having symptoms, can you talk a little bit about what they might be feeling?
Dr. Brinkman: One problem might be aortic stenosis where the valve leaflets are thickened, calcified, don’t open well, and they’ll have fatigue Sometimes they’ll feel like they’re going to faint, occasional chest pain, and that can be a severe problem. That usually prompts a echocardiogram and referral to my office. The other problem could be a leaky valve, someone who the leaflets don’t come together well; there’s poor apposition between the leaflets. That can also cause fatigue and heart failure-type symptoms, leg swelling, and that’s something we can also help with.
Adam Pick: It sounds like, Dr. Brinkman, this is a very serious condition and something that should be actively monitored. I got to ask you the question I’m guessing folks – could this be a fatal form of cardiac disease?
Dr. Brinkman: Well, it can be. Valvular disease tends to come on slowly and insidiously. It doesn’t tend to have an abrupt catastrophic failure such as aortic dissection, for example, but it can, especially with aortic stenosis. When you become symptomatic, we have data saying about 30% – there’s about a 30% mortality per year, and that’s why we feel strongly about helping people prevent that avoidable problem.
The only other thing I was going to add, if you have a leaky valve, aortic insufficiency we call it, your heart can become volume overloaded and dilate with time, and you go into congestive heart failure. Your legs swell, and it’s because the extra work your heart is having to do. It pumps blood out and a lot of it comes right back in the ventricle, so it’s having to work double-time. We fix the valve and your heart becomes more efficient.
Adam Pick: You’ve fixed a lot of valves out there and before we get to the treatment of bicuspid aortic valves, you brought up aortic dissection. Before we get ahead, put the cart – what’s the saying, the cart in front of the horse, can you maybe talk about how a bicuspid aortic valve might be related to an aortic aneurysm and ultimately to dissection?
Dr. Brinkman: They are related because the embryology is such that the development of the valve, your aortic root in the ascending aorta, which is the first part of the aorta, they develop together. The genes that are responsible for them are associated, so if you have an abnormal valve, many times your ascending aorta – the cellular architecture’s a little bit disorganized, and we feel it promotes aneurysm formation. Sometimes people debate over whether it’s the flow through the valve causing the aneurysm or is it the chicken or the egg kind of thing. The bottom line is they’re associated. As your aorta gets bigger, the stress on the wall is greater, and so that’s where people with bicuspid valve can have risk of dissection and rupture, which is a catastrophic problem you want to avoid.
Adam Pick: By catastrophic, you mean patients being rushed to the hospital, if that can happen. I’ve heard the stories of John Ritter, I believe, who suffered from dissection, and maybe Lucille Ball. This is something that – when a dissection happens, this is not just critical; this is nuclear for patients to get their arms around, correct?
Dr. Brinkman: Well yeah, I mean, John Ritter’s a great example because many times, it’s – he has a bicuspid valve which is working pretty well. He feels fine. He has an aneurysm which doesn’t cause any pain, and then it tears one day. You go from feeling fine to having a lot of trouble. Many times, the doctors in the ER are thinking one thing’s going on and it can be confusing. That’s why it’s good to follow this, get the proper tests, and to know what the problem is so we can address it in an elective manner but if it is an emergency, we can address it quickly and properly.
Adam Pick: Let’s talk about addressing the bicuspid aortic valve and potentially the associated aneurysm, and maybe we can do it in three different categories, if you will. It seems like the way that you identify the potential issues with the bicuspid aortic valve starts with almost aortic stenosis. There, you could have leaflets that are potentially calcified in which the valve is narrow. Can you talk about how you go about treating a bicuspid aortic valve that’s stenotic?
Dr. Brinkman: Well, like you said, the first step may be your doctor hearing a murmur and then they might get an echo. They’ll detect how much pressure it takes to push the blood out across the valve. We can measure the pressure underneath the valve and beyond the valve When the pressure gets to a certain level, we call it severe. We know that especially if you’re having symptoms, that is associated with heart failure and sometimes even sudden death. That justifies a valve repair or replacement.
With calcified valve leaflets like aortic stenosis, we usually can’t do a repair, per se. That requires replacement. Sometimes with the leaky valves, which we may talk about, we repair those.
Adam Pick: Yeah, there’s no doubt about it because five years ago, I didn’t really hear much about aortic valve repair, and it seems like there’s been this wonderful trend to reconstructing valves in a way that really wasn’t done before. Can you share a little bit about how you are repairing the aortic valve?
Dr. Brinkman: It’s much like what you see with a mitral valve. If you have good leaflet tissue there, we can re-approximate those leaflets together and make a working valve. If the leaflets themselves have calcium in them, like in aortic stenosis, it’s tough. Many times, people with a leaky aortic valve – the reason it’s leaking is the leaflets have pulled apart; the insertion points of the annulus of the valve has dilated. What we do is we do what’s call a re-implantation technique, which was pioneered by Tyrone David. We’ve had very good results with that. By bringing the leaflets in closer to each other and they have better coaptation. Rather than just barely touching, they come together nice in a position of prayer, almost. That’s what I learned from Duke Cameron; he taught me that. He’s like, “You want the leaflets like they’re praying, not just barely coming together.” You have a lot of coaptation.
Adam Pick: If I understand it right, by having that coaptation, that’s where the blood can’t leak back, right? If the valve leaflets are like this, the blood is going back and forth. Is that correct, Dr. Brinkman?
Dr. Brinkman: Yeah, I mean, if you can imagine, the leaflets aren’t really coming together, blood’s going to be shooting underneath. If they’re barely touching, it’ll be coming through. If they’re coming like this with a lot of coaptation, I mean, it’s tight. It’s tight. It’s going to be sturdy long-term. You don’t want to do a repair that’s just going to last one or two years. You want a repair that’s going to last 30, 40, 50 years, and that’s our goal. We don’t accept marginal coaptation in our repairs.
Adam Pick: Yeah, and it’s a great goal to set and achieve because you get durability You’re going to have very happy patients versus going in for reoperation after reoperation. Dr. Brinkman, we’ve talked about replacing the valves. We’ve talked about repairing valves. Your team, as I understand it, is working on some other complex procedures that also can bring about some fantastic durability for patients, including the Ross procedure Is that right?
Dr. Brinkman: The Ross procedure is a very good option in younger patients who don’t want to be on Coumadin. Traditionally, if we did a valve replacement in a younger patient, we’d put in a mechanical valve, which works well and that’s the gold standard in a lot of ways if you look at guidelines. However, the Ross procedure takes your own living valve, the pulmonary valve, and we move it into the aortic position, and that valve is alive. It can heal itself and can grow. It’s especially good with younger children. Up to the age of about 50 to 55, we’ll consider it. It’s a great option for someone who doesn’t want to be on Coumadin, who has an active lifestyle. It is a little bit more of a complex procedure and requires a center that is focused on it. We at the heart hospital in Plano have quite an experience of over close to 300 Ross procedures with very excellent freedom from reoperation out to 20 years.
Adam Pick: As you may know, Dr. Brinkman, I actually had a Ross procedure and I am familiar with so many patients, including Melissa Causey, who came down to the heart hospital to get a Ross procedure. She’s doing fantastic, and so thank you for all the pioneering that you and your team, including Dr. Ryan, have been doing for that procedure.
Now maybe we can talk about when the aneurysm comes into play and with a bicuspid aortic valve. Can you share maybe the different strategies and procedures you might use when you’re addressing those two conditions?
Dr. Brinkman: If someone has an aneurysm of the ascending aorta in the aortic root where the valve is seated, my first question is what’s the size of the aorta? Does it need to be replaced? What’s the quality of the tissue? If we think it does need to be replaced, then my next question is do I need to replace the valve? Can I repair the valve? If the leaflets are supple and not thickened and calcified, we will, many times, try and are frequently successful in repairing the valve. However, if the leaflets are not quality and not good, thinned out, have holes in them – we call them fenestrations – then we’ll move to a replacement. You may have a replacement with a biological valve or a mechanical valve. We can take a graft with a valve sewn into the end of that, and that’s called a Bentall procedure where we replace the root and the valve together. We can do that with a cow valve, pig valve, or a mechanical valve. Then of course, there’s the Ross, which is a root replacement with your own living tissue in there.
Adam Pick: The idea of this valve-sparing root is often hard for a patient to really understand that you want to keep the valve. You don’t want to replace it. Can you just real quickly shine some light on that for the patients as to why you want to do everything you can to keep that native tissue in the human body?
Dr. Brinkman: The valve leaflets themselves have layers of tissue that line it with a layer on the outside which decreases thrombosis. They have a supple living extracellular matrix, which is supple and moves. The cow valve leaflets and the pig valve leaflets will stiffen over time. They’re going to wear out on you if you live long enough. Your own valve will live – has the potential of definitely outliving the rest of your body, which is good, and that’s what we want. The Ross procedure, again, has living leaflet tissue in there, so it can last a long time, too. The cow valve works great but in most people, it’s going to last about 15 years, and that’s where you have to think about other scenarios. You need another operation or even a transcatheter valve replacement. I think it’s better to try and do something the first time and not have to do anything in the future if you can.
Adam Pick: Great point, and that was going to be one of my questions to you. As we conclude here, do you find that TAVRs, transcatheter aortic valve replacements, are now being used as either isolated valve-in-valve procedures or in situation where you have already done some kind of aneurysm repair? Can you still use a TAVR if you’ve done something like a Bentall procedure?
Dr. Brinkman: Yes, you can, especially if it’s a cow or a pig valve you have sewn in. If you’ve put a mechanical valve in, TAVR, you can’t really do that because the metal leaflets are blocking that. With a mechanical valve, they don’t wear out. It’s like a doorknob; it just keeps going. With a cow or a pig valve, 15 years down the road, if it’s a large enough valve that the surgeon put in, then it’s a great target for a TAVR. The key is to make sure that – the key for the surgeon to make sure is they put in an adequate sized valve. If you put in a small valve and try and blow up another valve inside of it, you may still have a blockage there, relative stenosis.
Adam Pick: Dr. Brinkman, I’ve done some research on you. I’ve looked at your profile. I think you’re now up over 2,000 heart valve procedures during your, what, 13-year career Is that about right?
Dr. Brinkman: Yep, it’s been good and busy, yeah.
Adam Pick: You’ve seen your fair share of patients who have had these procedures, and this is a question for the patients who are going to need a procedure in the future. What is your number one piece of advice for someone with a bicuspid aortic valve who will need surgery and might also have an aneurysm?
Dr. Brinkman: I think it’s important first to get in touch with a good cardiologist who understands valvular disease and knows what the guideline say about when to intervene and when not to. Also get in touch with – you may even want to talk with a specialist in thoracic aortic disease such as myself. A lot of my clinic is spent just reassuring people, telling them it’s okay. Go out and ride your bike and live your life because you have a small aneurysm. We’re going to follow it for years. That’s – if you do have an aneurysm which is large enough to intervene on, you need to have someone who knows when to intervene. I think my bigger advice is to get in touch with a cardiologist and/or surgeon who really knows this area and is into it.
Adam Pick: Fantastic advice because as I learned as a patient, you got to get a tribe around you. You got to get a village, a set of team – a set of clinicians who are specialists. Your family needs to get involved, your friends. It takes everybody coming together. Dr. Brinkman, thanks so much for your time today. On behalf of all the patients here at HeartValveSurgery.com, I want to thank you for all the great work that you’re doing at Baylor Scott & White in Plano, Texas. Thanks for your time.
Dr. Brinkman: Thank you, Adam, and thank you for your – the opportunity to talk to these patients and I appreciate your HeartValveSurgery.com





