Doctor Q&A: 5 Must-Know Facts About TAVR for Aortic Valve Patients
Written By: Allison DeMajistre, BSN, RN, CCRN
Medical Expert: Dr. Michael Deeb, Professor of Cardiac Surgery, University of Michigan Health
Reviewed By: Adam Pick, Patient Advocate, Author & Website Founder
Published: July 10, 2024
It wasn’t long ago that people with aortic stenosis only had one option: surgical aortic valve replacement (SAVR) with a new mechanical or bioprosthetic valve. Over the past twenty years, however, we’ve seen significant progress and technological advancements in minimally-invasive aortic valve replacement, most notably, transcatheter aortic valve replacement (TAVR).
The innovations we’re experiencing now are incredible, but they also create questions and potential uncertainty for anyone receiving news that they require an aortic valve replacement in the coming weeks or months ahead. When I had the opportunity to speak with Dr. G. Michael Deeb, the Inaugural Herbert Sloan Professor of Cardiac Surgery at the University of Michigan Health in Ann Arbor, Michigan, I was thrilled to ask him the most pressing questions about SAVR and TAVR coming from our patient community.
Dr. Deeb’s Key Learnings About TAVR
Here are important insights that Dr. Deeb shared with our community:
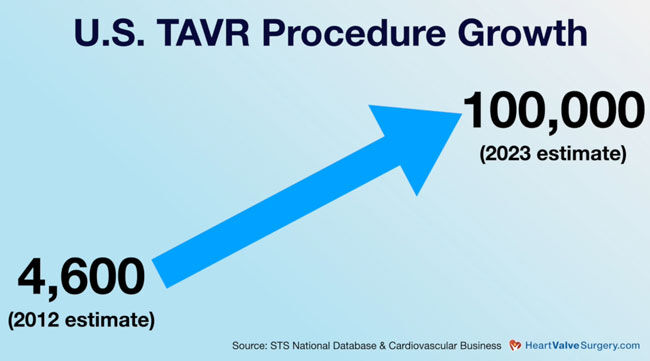
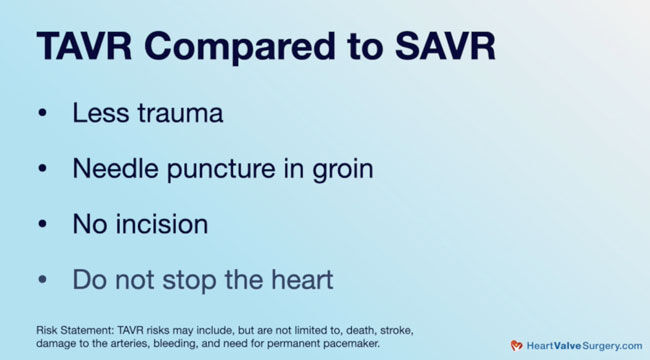
- With the tremendous growth in TAVR and over 100,0001 procedures already performed, I asked Dr. Deeb about the differences between TAVR and SAVR. “The biggest difference is the amount of trauma the patient experiences,” he said. “Whether fully invasive, partially invasive, or minimally invasive, open heart surgery is an open heart.” With that, Dr. Deeb described TAVR as a minimally-invasive puncture at typically in the groin (not an incision to the chest), and the medical team is not required to stop the heart during TAVR. The medical team watches images on a video screen as they pass a wire up through the artery. “The wire is like a railroad track,” Dr. Deeb said. “Over that wire, we have a hollow catheter as big as my finger; that’s the train. Then we have the valve, which is the passenger. The valve is in a circular wire frame, and inside are three leaflets made from the heart of a cow or a pig. As the valve is compressed, we slide it up and release it. It pushes the old valve up and away, and the old valve is never removed.” Like most procedures, there are risks to TAVR which may include, but are not limited to, death, stroke, damage to the arteries, bleeding and need for permanent pacemaker.
- Next, Dr. Deeb talked about the best candidates for TAVR. He told us that TAVR was initially only for older patients who couldn’t undergo the trauma of open-heart surgery. As time passed, TAVR was successful for the older patient population who were high surgical risk2. Before long, they were performing TAVR on intermediate-risk patients, and now, low-risk patients are also having the procedure. “Risk has nothing to do with it now,” he said. “It all has to do with lifetime management. When I see you, and you need an aortic valve, I look at your age, your medical condition, and how I can get you back on the normal survival curve. How can I get you to 85 years old with a minimal number of procedures, cumulative risk, and trauma?” Benefits may vary, for some patients, the Medtronic TAVR procedure risks may outweigh the benefits. Please talk to your doctor to decide whether this therapy is right for you.
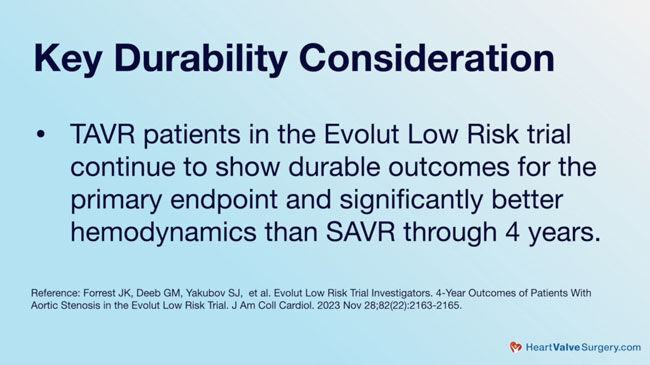
- Our patient community often asks about TAVR durability. Dr. Deeb said, “Valvular degeneration is quantified differently now.” He told us that when they only did surgical valves, they tracked patients until their valve deteriorated and needed a second surgery. “We called that durability,” Dr. Deeb said. “Now we’re following hemodynamics. (Hemodynamics and gradients are important to how your valve functions.) We follow the gradient and how hard the heart has to work when the valve begins to redevelop stenosis or a leak. Certain TAVR valves have better hemodynamics3 and less degeneration (dysfunction)4 than surgical valves.” (For more, see “Breaking News: New Medtronic Evolut Low-Risk TAVR Clinical Trial Results”.)
- Dr. Deeb said his best advice for patients considering a TAVR is to go to a multidisciplinary center of excellence and meet with the cardiologists and cardiac surgeons as a team. “They’re not advocating for surgery or TAVR. They’re advocating for what is best for you, what fits for you in that lifetime management,” he said.
The statements and information presented herein may be the opinion of the individual physician featured and is not intended to constitute medical advice.
Thanks Dr. Deeb and the University of Michigan Health!
Thank you to Dr. Deeb for answering our questions and sharing your experience and knowledge about TAVR to help our patient community make an informed and educated decision about aortic valve replacement! We also want to thank your team at the University Health in Ann Arbor, Michigan, for taking care of heart valve patients everywhere!
Related Links:
Keep on tickin!
Adam
P.S. For the deaf and hard-of-hearing members of our community, I have provided a written transcript of this video below.
References:
1 John D. Carroll, et. al, STS-ACC TVT Registry of Transcatheter Aortic Valve Replacement, Journal of the American College of Cardiology, Volume 76, Issue 21, 2020, Pages 2492-2516, ISSN 0735-1097.
2 Adams DH, Popma JJ, Reardon MJ, et al. Transcatheter aortic-valve replacement with a self-expanding prosthesis. N Engl J Med. May 8 2014;370(19):1790-8.
3 Forrest JK, Deeb GM, Yakubov SJ, et al. 4-Year Outcomes of Patients With Aortic Stenosis in the Evolut Low Risk Trial. J Am Coll Cardiol. Oct 18 2023.
4 Van Mieghem NM. Five-year bioprosthetic valve dysfunction after surgery or self-expanding TAVI. Presentation at EuroPCR. 2023.
Video Transcript:
Adam: Hi everybody, it’s Adam with heartvalvesurgery.com. We’re in San Antonio at the annual meeting of The Society of Thoracic Surgeons. I am thrilled to be joined by Dr. Michael Deeb, who is a professor and leading aortic valve specialist at the University of Michigan Health in Ann Arbor, Michigan. Dr. Deeb, it is great to see you and thanks for being with us today.
Dr. Deeb: Thank you. Thank you for inviting me.
Adam: We’re at this conference learning great information, all about valve disease. TAVR (transcatheter aortic valve replacement) is being talked about a lot. There’s been a lot of growth in TAVR. I think now we’re up over a hundred thousand cases. I’ve got to ask you, for patients who may not be familiar with TAVR, what are the big differences between TAVR and a surgical aortic valve replacement?
Dr. Deeb: I guess the biggest difference is the amount of trauma that the patient experiences. With open heart surgery, it’s actually open heart, whether it’s fully invasive, partially invasive, or minimally invasive. With TAVR, it’s a bee sting. Basically it’s a needle puncture in the groin, not an incision. We do not stop the heart. On a big video screen, we have images and we pass a wire up. The wire’s like a railroad track. Over that wire, we have a catheter as big as my finger, which is hollow. We slide that over. That’s the train. Then we have the valve, which is the passenger, and it’s in a circular wire frame and insider three leaflets made from the heart of a cow or a pig. The valve is compressed, slide it up and release it. It pushes the old valve up and away, and the old valve is never removed.
Adam: Wow, that’s fascinating, Dr. Deeb. Can you talk about who are candidates for TAVR?
Dr. Deeb: TAVR was first developed for those patients who had aortic stenosis but were older and couldn’t undergo the trauma of open heart surgery. Otherwise, if we could get them through the surgery without the trauma, would lead good longer lives. As time went on and it went so well for that patient population, we went from the non-surgical patients to those that had high risk, to moderate risk, to low risk. Risk has nothing to do with it now. It all has to do with lifetime management. What does that mean? When I see you and you need an aortic valve, I’m not looking at you saying, what procedure am I going to do now for you? I look at you and I say, based on your age, your medical condition, how can I get you from where you’re at back on the normal survival curve? How can I get you to, say, 85 years of age with a minimal number of procedures, a minimal amount of cumulative risk, and a minimal amount of trauma?
Adam: Dr. Deep, another question patients may have is, what is the durability of TAVR?
Dr. Deeb: Valvular degeneration is being quantified differently now. Previously when we just did surgical valves, we would track the patients to a point where their valve deteriorated and they needed a second surgery. We called that durability. Now what we’re doing is we’re following hemodynamics; we’re following the gradient; how hard the heart has to work when the valve is starting to feel and redevelop stenosis or develop a leak. It’s showing that, at a four year period, the hemodynamics in certain TAVR valves is better than in the surgical valve. The degeneration of that valve is less in TAVR as you go out four years.
Adam: It’s encouraging to hear that the data is coming out favorably thus far.
Dr. Deeb: It has.
Adam: A big question is, what advice might you have for patients out there who might be considering a TAVR?
Dr. Deeb: Always my advice is to go to a multidisciplinary center. Go to a center of excellence where you meet both the cardiologists and the cardiac surgeons in a multidisciplinary clinic at the same time, they’re working on the same team. They’re not advocating either surgery or TAVR. They’re advocating what is best for you, what fits for you in that lifetime management.
Adam: Dr. Deeb, on behalf of all the patients at heartvalvesurgery.com, patients all over the world watching this, thanks for everything you and your team are doing at the University of Michigan Health in Ann Arbor, Michigan. Thanks for being with me today.
Dr. Deeb: Thank you for inviting me.




