Doctor Q&A: How Is COVID-19 Treated?
Published: March 17, 2020; Page Last Updated: January 3, 2021
Since posting the 20 facts about the coronavirus, COVID-19, and heart valve disease, I’ve received many excellent questions about COVID-19.
One important question that many people are wondering right now is, "How is COVID-19 treated?" That said, I created this page to help answer that question.

As we have learned together, about 80% of patients will not require treatment as they may experience mild or no symptoms.
However, it is very likely that people we know will require some form of medical treatment for a COVID-19 infection. For this reason, I thought it would be helpful to learn about the current treatment protocols for COVID-19 to prepare you, me and all the people in our community.
 Dr. Allan Stewart
Dr. Allan Stewart
That said, I just spoke with Dr. Allan Stewart, a long-time supporter of HeartValveSurgery.com. Dr. Stewart has performed successful heart valve surgery on many patients in our community including Donna Herzek, Ray Pipher and Ed Abbate.
1. What is your number one recommendation for a patient who has tested positive for COVID-19?
When a patient tests positive for COVID-19, there are several important strategies to support recovery and avoid further spread of the virus.
First, DO NOT PANIC!!!
The overwhelming majority of patients who test positive for COVID-19 will have mild to moderate symptoms. Most patients will not experience a life-threatening illness.
If you have tested positive for COVID-19, it is important to get plenty of rest, stay hydrated and continue to eat. Often times, when we experience illness, our metabolism goes into overdrive (a hypermetabolic state) which can consume our muscle mass and leave us weakened. Having a food supply that is high in protein can mitigate these losses and help us recover. Protein shakes are another great way to increase our protein intake.
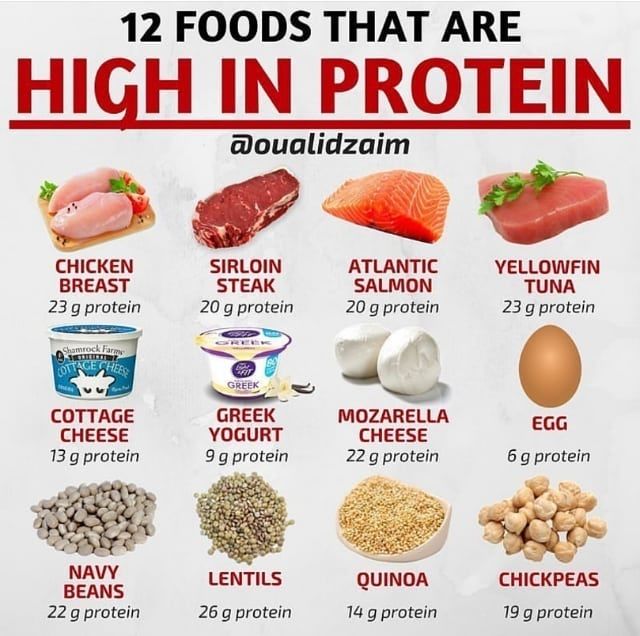
Above is a chart of foods that are high in protein – eggs, almonds, chicken breast, oats, cottage cheese, chick peas, Greek yogurt, milk, broccoli, lean beef, tuna, quinoa, salmon, lentils and pumpkin seeds. Specific to protein shakes, I’d recommend “whey” protein supplements shakes. Whey protein is derived from dairy foods that can help restore muscle mass.
The second recommendation is to self-quarantine.
During the rise of a pandemic, it is very important to self-quarantine and socially distance from others. Unless your symptoms are making you feel very sick, there is no need to visit an emergency room or a doctor’s office.

When you self-quarantine, please do everything you can to avoid contact with others. For example, if you need to order food or medicines, please pass the payment under the door. Then, wait until the delivery person leaves before opening the door and retrieving your goods.
The flu-like symptoms commonly associated with COVID-19 will most likely pass in a short period of time.
2. If a patient becomes symptomatic from COVID-19 what should they do?
A symptomatic patient should certainly seek treatment.
By symptoms, I mean worsening conditions that may include:
- difficulty breathing
- worsening fatigue
- increasing fever
- severe body aches
- nausea
- coughing and sore throat
It is helpful to call ahead and notify the treating facility (e.g. doctor’s office or emergency room) that you are coming. This may decrease your wait time and diminish the exposure risk to other patients. It will also be helpful for the care providers so they understand what specifically has worsened in your condition.
To help your medical team, you may want to demonstrate how your symptoms have progressed using comparisons. For example, you could say, “My temperature was X and now it is Y.” Or, you could say, “I was comfortably breathing before. Now, I can’t seem to catch my breath.” Or, you could share, “I noticed that my lips and fingers have become pale or appear a bit blue.” These comparisons may help your doctor start immediate and appropriate treatment.
3. Do most patients recovery from a COVID-19 illness?
Although this is a very confusing and scary time for most people, there is some positive news about COVID-19.
As we have seen across China, the vast majority of patients will fully recover from a COVID-19 infection. I want to repeat that. The vast majority of patients will fully recover from this coronavirus.
Additionally, patients may also be immune to a re-infection. As we have seen in recent reports, there is unlikely to be long-term consequences or any permanent lung damage.
4. What is the treatment process for COVID-19?
Unfortunately, at this time, there is no effective anti-viral medicine or vaccine for COVID-19.
Progress is being made every day. However, there is no documented treatment strategy, or cure, that has been proven effective yet.
That said, medical teams are supporting patients with various devices and techniques that are designed to support our bodies while we fight the virus. Those devices include ventilators, which are commonly referred to as respirators. A ventilator is designed to help patients breathe. The other technique for supporting the body during infection is ECMO, or extra-corporeal membrane oxygenation (see more below).
 A Patient On A Ventilator
A Patient On A Ventilator
It should be noted that ventilators and ECMO are not treatments for COVID-19. Again, there are no proven cures for this virus. The reason we use ventilators and ECMO is to support the body as the infection passes.
As I mentioned above… To help the body fight the infection, it is very important that patients get lots of rest, proper hydration, a high-protein diet, and symptomatic relief (lozenges, inhalers, Tylenol, etc).
5. What role does ECMO have during the COVID-19 treatment process?
ECMO (extra-corporeal membrane oxygenation) is essentially a temporary artificial lung. In cases of respiratory failure, ECMO (reserved for complete collapse of the functional lung capacity) will allow the blood to be filled with oxygen and relieved of carbon dioxide.
ECMO is performed at most heart institutes including all of our HCA facilities in Miami-Dade: Mercy Hospital, Adventura Medical Center and Kendall Regional Medical Center.
The procedure involves inserting a small catheter (typically in the large vein of the neck). This is accomplished by numbing the skin and using a needle, followed by passing a wire through the needle, and then a catheter. The special catheter has two tubes. One tube serves as the entrance port (the blood lacking oxygen) to the ECMO circuit. The other tube is connected to the exit tubing of the ECMO circuit (filled with oxygen rich blood). ECMO is somewhat similar to dialysis. However, instead of supporting the function of a deficient kidney, we are supporting the infected lungs.
It is important to realize that ECMO does not treat COVID-19. ECMO, when necessary, enables a critically ill patient to survive, when a ventilator is no longer enough support. In the small number of patients that may develop critical illness from COVID-19, the vast majority of these patients will be adequately supported with a breathing tube and the help of mechanical ventilation. In a small subset of these patients, the ventilator will not be enough. For these patients, ECMO may be required and has the potential to be a life-saving treatment.
During the H1N1 crisis, we saved many patients with this approach.
6. What thoughts do you have for people concerned about COVID-19?
I am quite worried about a patient population that has not been adequately addressed by the media. I am speaking about the young folks who vape. I have a suspicion that these people will be at increased risk for respiratory events with COVID-19.
Vaping is known to cause acute lung injury. That injury may allow the coronavirus to more deeply infect otherwise healthy lungs. This “one-two punch” may really debilitate our young population. My advice to these people is to put down the vape pen now. Or, forever if possible. But, AT LEAST, until this crisis passes.
For the rest of the population there is something called the 90:10 rule. 90% of our circumstances cannot be changed, but we do have control of the other 10%. We can be good members of society now and recognize that we live in a community where this virus will not discriminate based on gender, race, socio-economic status, or birthright.
Please listen to the recommendations and practice social distancing.
- Purchase what is required for your household but avoid hoarding supplies that other families may need
- Wash your hands frequently and definitely upon entry into the house or arrival to / from work
- Stay home when you are sick
- Come to the hospital only when your symptoms demand
Lastly… When spending time at home, consider playing a board game that does not have a screen or an “on/off” switch. Perhaps this is a time where families can re-discover actual communication and group activities.
Keep Learning About COVID-19 & Heart Valve Disease
To help you learn about coronavirus, COVID-19 and heart valve disease, you may also like:
- Heart Valve Surgery & COVID-19 Vaccines: 10 Facts to Know
- Free eBook: Advances in COVID-19 & Heart Valve Therapy
- Is Heart Valve Surgery an "Elective" Operation During COVID-19 Crisis?
- 5 Reasons We Are "Social Distancing" To Prevent COVID-19 Spread
- 20 Facts About Coronavirus, COVID-19 & Heart Valve Disease
- In Difficult Times... John & Larry Inspire Us
- COVID-19 Surgeon Roundtable: An International Perspective
- Inside the Operating Room: Dr. Allan Stewart Explains Heart Surgery
- CDC: Coronavirus Disease 2019 (COVID-19) Situation Summary
References:
- Washington Post: https://www.washingtonpost.com/health/2020/03/06/coronavirus-how-to-self-quarantine/
- Heartline: https://www.healthline.com/nutrition/20-delicious-high-protein-foods
- Steemit: https://steemit.com/health/@rohanmore/high-protein-food-daily






