Robotic Mitral Valve Replacement: What Should Patients Know?
Written By: Adam Pick, Patient Advocate & Author
Medical Expert: Robert Smith, MD, Chairman of Cardiovascular Surgical Services at Baylor Scott & White The Heart Hospital – Plano
Published: July 26, 2022; This post is sponsored by Abbott.
Over the past 20 years, the use of robots to perform minimally-invasive, mitral valve repair surgery has been harnessed by many leading cardiac centers. As a result, patients often ask me, “Can the robot be used to replace my mitral valve?”
In the past, my answer to that question was “no”. However, I recently learned that new innovations in heart valve replacement devices have enabled surgeons to perform mitral valve replacement using a robot. To learn more, I interviewed Dr. Robert Smith, the Chairman of Cardiovascular Surgical Services at Baylor Scott & White The Heart Hospital – Plano. As you may know, Dr. Smith is long-time supporter of HeartValveSurgery.com and has successfully treated many patients in our community including Gayle Ross and Greg Lybrand.
Key Learnings About Robotic Mitral Valve Replacement
Here are important learnings I jotted down during my interview with Dr. Smith:
- Mitral valves typically need treatment when a patient has severe mitral regurgitation or mitral stenosis. The patient can be symptomatic (fatigue, shortness of breath, leg swelling) or asymptomatic.
- If mitral valve disease is not treated – with a mitral valve replacement or a mitral valve repair – the disease can lead to serious health concerns including atrial fibrillation, heart failure and death.
- While there are multiple approaches (e.g. sternotomy, port access) for accessing the mitral valve, Dr. Smith prefers using robot-assisted heart surgery which provides patients several benefits from this minimally-invasive technique. Dr. Smith states, “Using the robot really limits the trauma that the chest experiences. The patient gets over surgery faster. The idea is I’m doing the same thing that I would otherwise do through a sternotomy and I’m doing it with less trauma, which means faster recovery.”
- To perform robotic mitral valve replacement, the devices used to replace mitral valves needed to evolve. New innovations include lower profiles and flexible materials. “Some of the things that have occurred is, number one, they’re very low profile. Instead of these really long arms, they’ve been really shortened,” states Dr. Smith. “The next thing is the material that they’re made of, the framework itself has become more flexible. We can fold these new valves flat, slip them in through that small rib space, and secure them back into the mitral valve area just as if we had done a regular procedure. Then, once we allow them to open, they spring open, just like we would have it if we had done an old time open replacement.”

Epic Plus Mitral Valve Replacement (Abbott)
- The durability of select, tissue valves is not compromised as a result of the new features which enable robotic mitral valve replacement. For example, the Epic Plus valve is a next generation valve built from a pre-existing tissue valve platform, the Epic valve, which has 96% freedom from reoperation after a 10-year period.
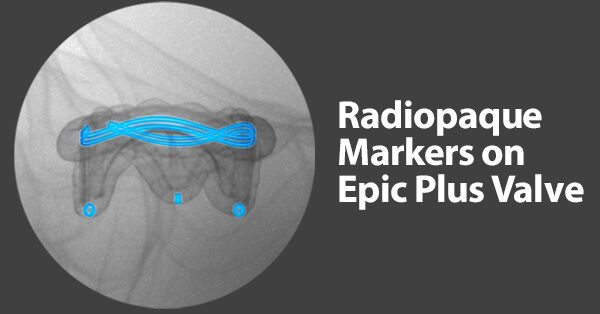
- As patients are living longer lives, next generation heart valve replacements, including the Epic Plus valve, have radiopaque markers that enable better visualization under X-ray should a patient need a future “Valve-in-Valve” procedure. These Valve-in-Valve procedures do not require any incision to the patient’s chest or ribs. “One of the things I’m really lucky to get to participate in is not only putting the valves in put also re-replacing them down the road through transcatheter procedures, which we do as a heart team,” states Dr. Smith.
- Dr. Smith’s advice to patients needing mitral valve surgery is to adopt a long-term and shared decision making approach with their surgeon and medical teams. Dr. Smith states, “Something I would recommend to all patients when they go see their surgeon to have this discussion is that that surgeon is ready and willing to listen to what the patient factors are that’s going to help them to determine what’s the right solution for them right then at that time and going forward, meaning are we going to have a plan for a long-term management and lifestyle management along with this.”
Many Thanks Dr. Smith & Baylor Scott & White The Heart Hospital – Plano!
On behalf of our patients, many thanks to Dr. Robert Smith for sharing his clinical experience and research with our community! Also, many thanks to the Baylor, Scott & White Team team for taking such great care of heart valve patients.
Related links:
- Cardiac Innovation: The Epic Plus Heart Valve Replacement
- See Dr. Robert Smith’s Interactive Surgeon Profile
Keep on tickin!
Adam
P.S. For the deaf and hard of hearing members of our patient community, I have provided a written transcript of this video below.
Video Transcript:
Adam Pick: Hi, everybody. It’s Adam with heartvalvesurgery.com. Today we have a very exciting surgeon question and answer session all about robotic mitral valve replacement surgery. I am thrilled to be joined by Dr. Robert Smith who’s the leading cardiac surgeon at Baylor Scott & White The Heart Hospital in Plano, Texas. During his extraordinary career, Dr. Smith has performed over 3,000 cardiac procedures with more than 1,500 involving some form of heart valve repair or replacement therapy. Dr. Smith, you and I have known each other for a long time. I just want to thank you so much for being with us today.
Dr. Smith: Adam, thanks for having me. I’m really excited to be with you and your patients who will be visiting you at heartvalvesurgery.com. This is a great opportunity to talk a little bit about heart surgery, something – I mean, you can get just about any topic in heart surgery, but particularly what we’re going to talk about today, I’m very excited about.
Adam Pick: Yeah, so we’re going to get all into robotic mitral valve replacement surgery, but first, Dr. Smith, for patients who may have recently been diagnosed, can you help them understand what is mitral valve disease?
Dr. Smith: It comes in basically two flavors: mitral valve regurgitation or mitral valve stenosis. Now, there’s a variety of severity within that but that’s the two basic issues that we’re dealing with. Regurgitation means a leaky valve. Stenosis means a tight valve.
Adam Pick: Dr. Smith, can you talk about some of the symptoms that a patient with mitral regurgitation or mitral stenosis might have?
Dr. Smith: Adam, I sure can. For both mitral valve stenosis and mitral regurgitation, probably one of the earliest symptoms that patients will experience is fatigue. It can be really insidious, creeping up on them. Oftentimes, I’ll have to ask their partner, spouse, is it really affecting them. I think the second biggest thing after we get from that is shortness of breath. Now, shortness of breath is oftentimes one of the things patients experience when they’re exercising or doing something. It may be getting to the top of the stairs and having to take that real big deep breath, like a sigh. It could be going out for a walk and not being able to get quite as far as you used to get. Unfortunately, as these disease processes continue to get worse, patients will feel worse, sometimes with swelling of their legs and a real inability to get through their day.
Adam Pick: Dr. Smith, these are no doubt debilitating symptoms. I’m curious to know. Are there any serious health risks for patients who have mitral valve disease?
Dr. Smith: That’s a great point to this. As the disease severity worsens, patients can not only develop these symptoms but real medical issues associated. Number one would be atrial fibrillation. This is a particularly bad one where patients’ heart rates can race really fast. They could almost feel like they’re racing but sitting in a chair. In addition, the heart muscle can weaken over time, causing heart failure. Ultimately, patients can succumb to this and it could lead to death. Lastly, in certain patients, they could be at an increased risk for endocarditis, which is an infection of the heart valve, which is also associated with death.
Adam Pick: Dr. Smith, given the seriousness of the symptoms and the potential health risks, I have to ask you. How do you go about treating mitral valve disease?
Dr. Smith: In trying to determine what’s the right treatment, I really have to know what is the problem. Is it regurgitation or stenosis? That helps me decide, is this going to be a repair of the valve where we really leave all the native structure of the valve and just support it and put it in the right place? Is this valve so broken that I need to replace it? In that case, and in both cases really, we have another decision to make, which is what’s the right approach to get to the valve?
For patients who only have a mitral valve problem or have a mitral valve problem and another valve problem like a tricuspid valve problem which can oftentimes be associated with mitral valve disease, we usually can use minimally-invasive techniques to get there. Minimally-invasive techniques can sometimes mean a small incision in the side of the chest, or and more commonly what I do, is robotic surgery where we make little small port incisions in the chest and a small incision down the groin for the heart lung machine. Through that, we can do the entire procedure, either a repair or a replacement, and get somebody’s valve taken care of.
Adam Pick: Dr. Smith, I’ve got to ask you. There’s lots of different approaches out there. You mentioned some of them: robotic and minimally-invasive and traditional sternotomy. I’m really curious to know. When it comes to the robot, what is it from your perspective, the surgeon’s perspective, that’s advantageous for you?
Dr. Smith: Adam, when I use the robot, the real big piece for the patient is the fact that, while we put little small incisions on the chest, the ports that go through the rib spaces don’t really widen the rib spaces. It’s so that really limits the trauma that the chest experiences. What does that really mean for the patient who’s undergoing surgery? He’s getting over surgery faster. The idea here is I’m doing the same thing that I would otherwise do through a sternotomy or through a port access, which is the small incision approach, and I’m doing it with less chest hole trauma, which means faster recovery. The reason we can do this is these ports through them those arms come in where the instruments are attached. There’s, first off, amazing visualization. It’s high def, 3D. The instruments come with little wrists on them so I’m basically performing the same wrist maneuvers that my hands would make on the end of an instrument deep inside of the chest.
Adam Pick: Dr. Smith, it’s great to hear about the advantages not just for the patient but also for you as you perform robotic mitral valve therapies. I want to back track. You mentioned earlier that you performed not only mitral valve repair procedures using robots but robotic mitral valve replacement. This is really new news to me. I had heard for many years about the FDA approval for repair, but can you talk about the evolution of the utility of the robot for replacing mitral valves?
Dr. Smith: The issue is sometimes a mitral valve repair, despite all of your best intentions, is not going as well as it should for the patient to provide a durable relieve of the regurgitation. Then you need to think about, hey, I need to put in a replacement here. If that’s the case, I don’t want to stop a procedure, take the robot out, and change to a port access approach or a sternotomy approach. Really, the valves are pretty small. I can put it in through a little side port between the ribs and not really have to convert anything, maintain the same approach and the same limited chest hole trauma, and the patient can get over it just as well.
We’ve just incorporated this into our practice where we do a fair number of mitral valve replacements in patients who are not good candidates for replacement. Now we just use the robot for that as well. There’s been some additional advantages to that for the patients, yes, but along with that you have to have other tools. I’ve got the robot tools but the valve companies had to come along and improve the way the valves work.
Adam Pick: Dr. Smith, this is fascinating. Let’s talk a little more about that. How have the next generation valve replacement devices enabled you to perform these mitral valve replacements robotically?
Dr. Smith: As we’ve really advanced the way that we get to the heart, now we’re in the robotic stage of things, the valves themselves had to improve over time in order to allow us to get them through this small rib space that’s there to minimize chest hole trauma. Some of the things that have occurred is, number one, they’re very low profile. Instead of these really long arms, they’ve been really shortened. The next thing is the material that they’re made of, the framework itself has become more flexible. We can fold these guys flat, slip them in through that small rib space, and secure them back into the mitral valve area just as if we had done a regular procedure. Then once we allow them to open, they spring open, just like we would have it if we had done an old time open replacement.
Adam Pick: Dr. Smith, one of the big considerations that patients have is durability of valve replacements. I’m just curious to know. Is there any tradeoff here when you go minimally-invasive using robot and some of these newer heart valve replacement devices?
Dr. Smith: Adam, as far as the way we approach the heart, that part doesn’t make a difference as far as how the valve is going to last. Valves generally come in two basic flavors. The mechanical valve, which is a really well tested valve for durability, is one we oftentimes use in younger patients. Now, those valves, the downside, Adam, is you have to use a fair amount of blood thinner. Tissue valves, when we look at the long-term, they don’t really require the blood thinner, specifically for the valve, except for the first three months.
We’ve also had considerable improvements in the way that they design those valves, including anti-calcifying agents to try to make the tissue themselves last longer. When we take, for instance, the epic valve, which is a pig valve, those valves, when we look at over about a ten-year period of time, 96% of patients would expect to have freedom from structural valve deterioration. What that means is, hey, I don’t really need to go in there and replace that valve because it looks almost like it did when I put it in.
Adam Pick: Dr. Smith, that’s amazing to hear about the low incidents of reoperation for the epic plus valve. I understand that there is also some other new innovations for that specific valve if by chance a patient needs some kind of reintervention down the road. Can you talk a little bit about that?
Dr. Smith: One of the really great things about the population at large is we’re living longer. Even those patients who have had previous valve replacement surgery are living longer. The idea is, can we manage this valve over time? One of the things I’m really lucky to get to participate in is not only putting the valves in put also re-replacing them down the road through transcatheter procedures, which we do as a heart team. The valves themselves now with this idea in line of, hey, this valve is not what God gave you. It’s not going to last as long as what you originally had, but what can we do to manage this? They put some markers in there so that when we’re putting a transcatheter valve in, which means the valve that would go in through the vein of the leg, come over and cross over the inside of the heart, and we deposit that valve right where the other one is. We use those markers to help position it right where it needs to be.
Adam Pick: Dr. Smith, that is fantastic for the patient. Are there any other advantages that patients should know about when it comes to a transcatheter valve and valve procedure?
Dr. Smith: There sure are. First off, it’s a heart team approach, which often times means there’s a cardiac surgeon, a cardiologist, and an imaging specialist all involved, which means you’re getting three minds involved in placing this one valve. The big thing that the patient notices, because that’s all happening in the backend or in the midst of the procedure, is they see a poke hole in the groin and they’re going home the next day. They usually get an echo before they leave that confirms, hey, the valve is looking good, but the overall experience is a much shorter one than the original surgery ones.
Adam Pick: Dr. Smith, it’s great to hear three minds are working together on a transcatheter valve that requires no incision to the patient’s chest or ribs. Thank you and your team for what you’re doing there at Baylor Scott & White. I guess one of the big questions that I have for you is, what is your number one piece of advice for a patient considering a mitral valve replacement procedure?
Dr. Smith: When a patient comes in, we’re going to have a discussion about mitral valve replacement surgery. Something I would recommend to all patients when they go see their surgeon to have this discussion is that that surgeon is ready and willing to listen to what the patient factors are that’s going to help them to determine what’s the right solution for them right then at that time and going forward, meaning are we going to have a plan for a long-term management and lifestyle management along with this. That’s something we get from the patient. You should come out with a shared decision at the end of that visit of what you’re going to do, either surgery with an idea of transcatheter purchased down the road or an idea of maybe a mechanical valve and anticoagulation. You the patient are very much the centerpiece of anything we discuss in the office.
Adam Pick: Dr. Smith, that is great advice. I hope the patients really listen to that idea of a shared decision with your medical team. As always, Dr. Smith, I want to thank you for taking time away from your very busy practice there at Baylor Scott & White The Heart Hospital in Plano, Texas. Really enjoyed having you with us today.





