Medical Breakthrough: Epic Plus Tissue Valve Gets FDA Approval
Written By: Adam Pick, Patient Advocate & Author
Medical Expert: Kenith Fang, MD, Chief of Cardiothoracic Surgery at Banner University Medical Center Phoenix
Published: June 2, 2022; This post is sponsored by Abbott.
Big news!
The lifetime management of heart valve disease has become a critical consideration for patients who want to live longer, more active lives. As a result, patients needing heart valve replacement surgery are asking important questions like, “What is the durability of my tissue and mechanical valve options?”, “Will I need multiple heart valve operations during my life?”, and “Can I undergo a Valve-in-Valve procedure should my first heart valve replacement fail?”

Given these questions, we are happy to share that the Epic Plus tissue valve recently received a Food & Drug Administration (FDA) approval. So you know, the Epic Plus valve is the “next-generation” of the Epic valve which has already been implanted in over 250,000 patients since 2008.
Why Are Heart Surgeons Excited About Epic Plus?
In our discussions with leading cardiac surgeons, we witnessed a unique excitement for the new Epic Plus valve.
To learn more about the Epic Plus tissue valve which does not require the use of blood-thinners, we interviewed Dr. Kenith Fang, the Chief of Cardiothoracic Surgery at Banner University Medical Center Phoenix in Phoenix, Arizona.
Key Learnings About the Epic Plus Valve
Here are several key points made by Dr. Fang about heart valve disease and the Epic Plus valve:
- Heart valves manage blood flow through the heart in one direction. Patient problems may occur if heart valves become narrow (aortic stenosis) or leak (mitral regurgitation).
- Patients may experience symptoms including chest pain, shortness of breath and dizziness. If left untreated, heart valve disease can be fatal. For example, 50% of severe aortic stenosis patients who do not get treatment die just 24 months after the onset of symptoms.
- There are different types of heart valve replacements. Biological valves made from pig or cow tissue typically last 10 to 15 years and do not require the use of blood thinners (e.g. warfarin) to prevent blood clots. Mechanical valves are made from durable materials (e.g. pyrolytic carbon) that are designed to last forever but require patients to permanently use blood thinners to prevent clots.
 Valve-in-Valve Procedure
Valve-in-Valve Procedure
- Dr. Fang suggests that the development of “Valve-in-Valve” technologies can extend the lifetime use of tissue valves as new valves can be inserted into failing valves without an incision to the patient’s chest or ribs. “If you outlive a tissue valve, you normally need open heart surgery again,” states Dr. Fang. “Now, we have transcatheter technology that allows us to put a new tissue valve inside that old pig or cow valve through the groin with no incision to the patient’s chest or ribs. You can go back to living your normal life very quickly after that.”
- It is important to note that there are some surgical heart valve replacements that are (i) not designed for and/or (ii) not implanted properly to enable the use of Valve-in-Valve procedures. Dr. Fang states, “There are some valves that are more amenable for Valve-in-Valve therapy. Other valves are not.”
- According to Dr. Fang, the Epic Plus valve made by Abbott is designed to accommodate Valve-in-Valve therapies so that patients can enjoy the benefits of tissue valves without needing a second open heart surgery.

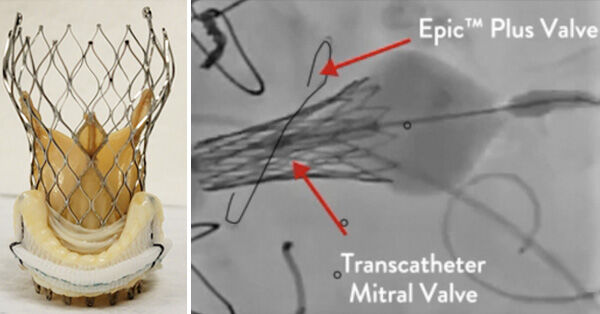
- One of the new features on the Epic Plus tissue valve is radiopaque markers. Radiopaque markers enable medical teams to better see and place transcatheter valves during a Valve-in-Valve procedure. “One of the main changes to the Epic Plus is really making that valve more visible under radiology, under x-ray,” states Dr. Fang. “During open heart surgery, I can see exactly what I’m doing. When we use catheter-based valves, we really need to see it not with our eyes in the setting of open-heart surgery, but we need to be able to see the valves with an x-ray machine because we’re doing things with catheters.”
- Another new feature of the Epic Plus valve is the ability to “fracture” the valve during a Valve-in-Valve procedure. As Dr. Fang explains, “We can take the Epic Plus valve and crack it open so that we can get a bigger valve inside the Epic Plus valve to prevent a valve that’s too narrow and does not allow blood to flow properly.”
- For enhanced durability, the Epic Plus valve also utilizes anti-calcification treatments on the valve tissue to reduce calcium build-up. “We can prolong the longevity of these valves, “ states Dr. Fang, “Maybe 10 to 15 years or maybe beyond that, based on some of these new technologies.”
- Dr. Fang’s advice for patients needing a heart valve replacement is to find an experienced heart surgeon who is very thoughtful about the lifetime management of heart valve disease. Dr. Fang believes it is critical that patients speak with a surgeon that understands new technologies (e.g. Valve-in-Valve procedures) that can enhance the patient’s quality-of-life and prepare the patient for multiple heart valve operations if needed.
New Educational Microsite Launches for Epic Plus!
To help patients learn more about the Epic Plus valve, we just launched an interactive microsite with educational videos, a free patient eBook, an Epic Plus surgeon finder and more.
Click here to experience the Epic Plus Educational Microsite for patients.
Keep on tickin!
Adam
P.S. For the deaf and hard of hearing members of our community, I have provided a written transcript of my interview with Dr. Fang below.
Video Transcript:
Adam Pick: Hey, everybody. It’s Adam with heartvalvesurgery.com. Today we have a very special surgeon question and answer session all about the advances and innovations in heart valve replacement devices for the lifetime management of heart valve disease. I am thrilled to be joined by Dr. Kenith Fang who’s the chairman of the department of cardiovascular services and the chief of the division of cardiothoracic surgery at Banner University Medical Center Phoenix in Phoenix, Arizona. During his extraordinary career, Dr. Fang has performed thousands of cardiac procedures of which many involved heart valve repair and heart valve replacement surgery. Dr. Fang, it is great to see you. Thanks so much for being with us today.
Dr. Fang: Adam, thank you so much for the invitation. It’s great to be part of the heartvalvesurgery.com community.
Adam Pick: Yeah, so let’s dive into it, Dr. Fang. To start, a big question that patients have, which is why might I need to have my heart valve replaced?
Dr. Fang: This is something I explain to patients all the time. Your heart’s a pump. This is all it does all day long. The valves in the heart is like a valve in any other device. Because without the valve, your heart will know no idea about am I pumping forwards or backwards. The valve is what directs blood flow in one direction and one direction only, if it’s functioning properly. Just like a valve in any mechanical device, one of three things can happen. It can not open properly. We call that stenosis. It can leak and not close properly. We call that insufficiency or regurgitation. Quite often, you have a combination of the two, but usually one or the other predominates, whether it’s stenosis or regurgitation.
Adam Pick: Dr. Fang, thanks for the explanation of valve disease and why a patient may need a heart valve replacement. Can you talk about some of those symptoms and health risks for people with valve disease?
Dr. Fang: When people have valve problems, it may be mild to begin with, but eventually over time, not all of them but a lot of them will become severe. When these valve problems become severe, you can get a large variety of symptoms depending on the type of valve that’s problematic. Let’s use the example of aortic valve. When an aortic valve becomes not open properly, i.e. aortic valve stenosis, that can lead to very serious complications. If left unchecked, you can actually die from something like this. Aortic valve stenosis are associated to something called sudden cardiac death. That means that you can really pass out one day and never wake up again. We know that people with severe aortic valve stenosis, as soon as they have the very first symptoms, and those three common symptoms are chest pain or pressure. You can get shortness of breath and fatigue. You can also have some dizziness and you can pass out, what we call syncope.
When patients have any one of those symptoms and they have an echo that shows they have severe aortic valve stenosis, if those patients decide for whatever reason that they don’t want to have surgery, you take 100 of those patients, you take them out to two years. If those 100 patients do not do anything about these problems, less than 50% of them will reach two years. That means that 50%, one out of two, will die in that span of time. This is not something that you want to neglect because it’s something that can be fixed if treated appropriately and time is of the essence.
Adam Pick: Dr. Fang, we definitely want to start talking about the treatment of these diseases given that death can be a result from them. Can you help patients understand what are the different treatment options if I need a heart valve replacement?
Dr. Fang: A traditional therapy for this is open heart surgery. Open heart surgery is a very broad category. Basically, we are operating on your heart. We’re putting you on a heart lung machine where we are opening up the heart to get access to the valve. That is traditional therapy. There’s a lot of nuances right now. We have catheter-based valve therapy where we can really put a valve inside your valve, the aortic valve, with a puncture in the groin where you could go home the next day. That’s not for everybody. If you have a mitral valve problem, a tricuspid valve problem, right now the main stay of therapy for that is really surgery still.
Now, having said that, surgery is no different than it was done 10 years ago, 15, 20 years ago, 30 years ago, but there are some nuances now. That nuance is that with the availability of transcatheter valves, we know that treatment options will be different in the future. When we do open heart surgery for these valve problems, i.e. the mitral and tricuspid valves, I think it’s important for your surgeon to understand that you need a plan today so you have better options in the future.
Adam Pick: Dr. Fang, I love hearing that you’re thinking about the entire lifetime management of valve disease, not just a single event for a patient. Because we know patients can be younger with valve disease. I’m curious to know, though. What would be an example of some of these nuances and techniques that you’re using to plan for the lifetime management of valve disease?
Dr. Fang: Now, normally, if I do a mitral valve operation on you, for example, you’re a young person. Chances are you’re going to outlive a valve that I put into you, especially if I chose to use something called a tissue valve, which is a pig valve or a cow valve. If you outlive that valve, normally you have to have open heart surgery again. Now we have new technology that allows us to put a new valve inside that old pig or cow valve, again, with just a stick in the groin, very real recovery time. You can go back to living your normal life very quickly after that.
If what is done during the original operation is not standard for a valve in valve or not geared toward a valve in valve in the future, it can make it either very difficult or impossible in the future. What do I mean by that? There are different types of valves that surgeons can use to replace your valve. There are some valves that are more amenable for what we call valve in valve therapy and other valves that are not.
Adam Pick: Dr. Fang, I love learning about valve in valve therapies and the innovation going on there. I’m curious to know. Were there any innovations that had to happen for the devices that would give you the opportunity to think about the long-term planning of valve in valve procedures?
Dr. Fang: You bring up a great point. There is obviously just an incredible amount of talent and direction with innovation inventions in these new transcatheter valves. We’re trying to figure out ways to be able to fix your valve without open heart surgery to allow you to get back to doing everything you want to do as soon as possible.
Now, not only is that technology changing things in the future for transcatheter valves, but that technology also exists right now for surgical valves that we put in. For example, there’s a valve called the Epic valve made by a company called Abbott. They just got FDA approval for something called the Epic Plus valve. This Plus is literally a change in the design in the existing pig valve that we use today to make that able to accommodate a valve in valve transcatheter valve so that your second operation is more likely to be successful with, again, just a stick in the groin so that you don’t have to have open heart surgery again. I think that kind of technology is really changing the future and also what’s happening today.
Adam Pick: Dr. Fang, if I’m a patient, I’m really curious now. Can you talk about some of those advances in the Epic Plus valve?
Dr. Fang: Adam, absolutely. One of the main changes to the existing Epic valve with the Plus is really making that Epic valve more visible under radiology, under x-rays. With open heart surgery, I can see exactly what I’m doing. When we use these catheter-based valves, we really need to see it not with our eyes in the setting of open heart surgery, but we need to be able to see this with an x-ray machine now because we’re doing things with catheters. To make that valve more visible is clearly something that would make a future valve in valve more successful.
Additional things are such as trying to make it so that the valve is easier to open up, fracture open. For example, when we put a valve in, we’re putting a valve inside a valve. That’s how these transcatheter valve therapies work for valve in valve. As you put something inside something, you’re going to realize that the caliber or the opening of that valve is going to get smaller. If we can put something in and make the older valve bigger by breaking it and pushing it out, then I could put in a bigger valve and not have the constraints of a hole that’s too small. One of the things they’ve done that’s very innovative is they allowed for what’s called fracturing of the valve. We can take that valve, more readily crack it open so that we can get a bigger valve on the inside of that valve to prevent a valve that’s too narrow and not allowing blood to flow through properly.
Adam Pick: Dr. Fang, love learning about that. I’ve got to ask. Patients are always curious to know about durability. Are any of these next generation valves, like the Epic Plus, doing anything to enhance durability?
Dr. Fang: It’s a question I get almost every patient ask me about. One of the talks I have is the difference between what we call mechanical valve and a tissue valve, which is the pig and cow valves typically. Mechanical valves are great in the sense that they can be very durable for 50 years. I’ve told people if you have a mechanical valve, in theory, if you lived to 130, that valve will last until you’re 130, but the problem with the mechanical valve is that you have to be on blood thinner called Coumadin, Warfarin every day for the rest of your life. A lot of people are very against that for obvious reasons.
Now, with the tissue valves, there is technology that’s changing the tissue valve, the pig and cow valves. The way they’ve changing that is that they’ve realized with the failed valves over the last several decades that they tend to fail because they have calcium impregnated. Our calcium that we have in our body will tend to not reject the valve but they will tend to have that calcium clean out those leaflets. It’s the calcium that destroys those valves over time.
The typical life expectancy right now for most of these valves, depending on which study you look at, is usually around 10 to 15 years. That’s what I tell most of my patients. We’re looking at technology to try to minimize the amount of calcium impregnated into these leaflets, i.e. anti-calcification treatment of these valves. We’re hoping that by doing these anti-calcification treatments, we can prolong the longevity of these valves, hopefully beyond that 10 to 15 years, maybe 10 to 50 years or maybe beyond that, based on some of these new technologies.
Adam Pick: Dr. Fang, thanks so much for that response. I’ve got to ask you. What is your number one piece of advice for patients who may need that first time heart valve replacement?
Dr. Fang: I think that’s a great question and a very important question. The reason why I think it’s important is that, unlike a lot of the heart pathologies that the average heart surgeon deals with, valve pathology is unique in the sense that it typically occurs over a long period of time, years. Most of my patients have known that they’ve had valve problems and that eventually they will need to have surgery. That time, unfortunately, creeps up on them and they have to have surgery.
When you find out that you need to have valve surgery, you have that time to investigate, not only the pathology and what it means, but also more importantly, find the right surgeon that can do your operation. The average heart surgeon, in particular for mitral valve pathology, doesn’t do a lot of mitral valve surgery. You don’t want that guy or that woman that only does maybe about five a year, ten a year. You want that person that does a lot of them per year. That’s where that expertise comes, especially for mitral valve.
When we do mitral valve surgery, we’ve talked about mechanical valve versus tissue valve, most people want a tissue valve. If you’re going to have that tissue valve and you’re having your surgery, not at 80-something years old but in your 40s, in your 50s, in your 60s, then that’s where this concept of lifetime management of valve pathology comes in. You need to make sure that you find not only a surgeon that understands and does a lot of mitral valve surgery. You need someone that understands all this new technology so that they can alter potentially the way they do your surgery today to make it more likely for this new technology in the future can accommodate what you have right now. The type of surgery that person does for you can be very important in that regard. Lifetime management goes into the realm of the surgeon and you need to make sure that you have the surgeon that understands that.
Adam Pick: Dr. Fang, fantastic advice. On behalf of all the patients at heartvalvesurgery.com, thanks for taking time away from your very busy practice there at Banner University Medical Center Phoenix and sharing all these wonderful insights with us. We can’t thank you enough.
Dr. Fang: Adam, the honor is mine. I’m so appreciative of the invitation to participate in this today. I think that what we do as patients in deciding what is going to be done with us as our own patient advocate is very important. I’m saying we because I am a patient as well. I’ve had all my own medical issues. When you’re your own patient advocate, you do the research. You find out what’s important. You make sure the person taking care of you knows what’s going on, is updated on all the nuances of this incredibly fast changing world of valve therapy. If you could do that, you’re going to increase your changes of having a good outcome today as well as into the future.





