Breaking Research: 4D Flow MRI Predicts Aneurysm Risk in Bicuspid Aortic Valve Patients
Written By: Adam Pick, Patient Advocate, Author & Website Founder
Medical Expert: Michael Markl, PhD, Professor and Vice-Chair of Research at Northwestern Medicine
Published: September 28, 2021
Bicuspid aortic valve disease is one of the most common forms of congenital heart disease impacting between 1% to 2% of the population. Interestingly, some patients with bicuspid aortic valves develop aortic aneurysms, a swelling (or bulging) of the aorta than can lead to life-threatening situations. Other bicuspid aortic valve patients, however, never develop an aneurysm.
For that reason, many patients and physicians have wondered, “Is it possible to create a diagnostic test for bicuspid aortic valve patients that can predict whether-or-not a patient is at risk for an aortic aneurysm?”
Here’s the wonderful news… I am thrilled to share that a diagnostic test for predicting aorta dilation in bicuspid aortic valve patients now exists!!!
Thanks to innovative research from the Bicuspid Aortic Valve Program at Northwestern Medicine, a team of scientists, surgeons, researchers, cardiologists and imaging specialists are using 4D Flow MRI technology to identify a new “biomarker” to predict aorta dilation in bicuspid aortic valve patients. In this video, we interview Dr. Michael Markl, Vice Chair and Professor of Research at Northwestern Medicine, to learn how 4D Flow MRI technology can help doctors better manage the potential risk of aortic aneurysms in bicuspid aortic valve patients.
Key Insights About 4D Flow MRI & Aorta Dilation for Patients
Dr. Markl shared several important points during this interview that I want to highlight for our patient community:
- In his role at the Bluhm Cardiovascular Institute at Northwestern Medicine, Dr. Markl leads a multi-disciplinary team that develops new imaging technologies to help physicians better manage and treat heart disease and stroke.
- 4D Flow MRI is a novel imaging technology developed at Northwestern Medicine. With 4D Flow MRI, physicians can measure blood flow through the heart and the aorta of patients.
- Bicuspid aortic valves are malformed, two-cusp valves that can lead to serious symptoms (shortness of breath, fatigue, chest pain, dizziness) and complications (aortic aneurysms, heart failure and death) for patients. A normal aortic valve has three cusps.
- Historically, cardiologists and cardiac surgeons have been puzzled by the development of aortic aneurysms in patients with bicuspid aortic valves. Dr. Markl states, “One of the questions that always puzzled cardiologists and cardiac surgeons is, ‘Why is it that one group of BAV patients develops complications while another group of BAV patients do not have complications?’ This new study addresses this important question.”
- In this longitudinal study, the Northwestern Medicine team found that 4D Flow MRI can help identify a unique biomarker known as “wall shear stress”. This biomarker can predict the potential development of aortic dilation in a patient. Dr. Markl states, “It turns out if you have more wall shear stress in your aorta, you’re at higher risk for aortic dilation. This may eventually lead to the need for surgery and valve repair in those patients.”
- Wall shear stress measures the drag force of blood on the aortic wall. That force can ultimately cause disease and aortic complications.
- The uniqueness of this study is that Northwestern Medicine was able to measure wall shear stress “in vivo”, in patients, using 4D Flow MRI.
- The application of 4D Flow MRI and the wall shear stress biomarker is very helpful for heart teams to manage patients with a bicuspid aortic valve. Dr. Markl states, “It really is a tool to hopefully better manage patients and plan ahead for the remainder of their lives. Bicuspid aortic valve is a birth defect. It’s something you carry with in your life. You really want to plan ahead and manage that care as efficiently as possible for the patient.”
Congratulations to Dr. Markl & Northwestern Medicine!!!
On behalf of the patients at HeartValveSurgery.com – especially the bicuspid aortic valve patients – I’d like to extend a big-time “Congratulations!!!” to Dr. Markl and his entire team at Northwestern Medicine for this exciting and very encouraging research! I imagine this new application of 4D Flow MRI and wall shear stress will help many, many, many patients in the future!
Keep on tickin!
Adam
P.S. I have provided a written transcript of this video interview below.
Video Transcript:
Adam Pick: Hi, everybody, it’s Adam with heartvalvesurgery.com, and this is a special research alert all about a new innovation in cardiac imaging for bicuspid aortic valve patients. I’m thrilled to be joined by Michael Markl, who’s a Professor and Vice-Chair of Research at Northwestern Medicine in Chicago, Illinois. I am so excited to learn about all the exciting things coming out from your research but first, a question for you, Michael. What is your role there at Northwestern Medicine?
Michael Markl: Yeah, thanks, Adam. I’m actually a physicist by training, and I’m now a research professor in the Department of Radiology at Northwestern University. I had a research group, and our goal is really to develop new imaging technology for the improved diagnosis, management, and therapy management of patients with heart disease and stroke. Heart valve disease and heart valve surgeries is a very important area of research to us.
Adam Pick: Let’s talk about the new research that was just published in the Journal of American College of Cardiology, the cardiovascular imaging sub-journal What were you studying?
Dr. Michael Markl: It’s about applying one of our novel imaging technologies that we’ve developed at Northwestern that we call 4D flow MRI for patients with bicuspid aortic valve disease. Maybe to give you a little bit of background. Bicuspid aortic valve disease is the most common birth defect in the heart. It affects 1 to 2% of the population. Now what’s interesting about bicuspid aortic valve disease, or BAV disease, is that it can lead to serious complications such as dilatation of the aorta, which might then lead to the need for surgery. What’s really interesting here is although all the patients are born with the same heart defect, not everybody develops that kind of complication.
One of the questions that has always puzzled cardiologists and cardiac surgeons is why is it one group of patients develops complications and why is it another group of patients doesn’t. This study actually goes at addressing this question. The hypothesis is the abnormal valve causes changes in blood flow in the aorta.
Adam Pick: Michael, thanks for the context of BAV and the issues that can be happening with the aorta and 4D flow MRI. Let’s talk about that. Can you share some of the findings that came out of your research?
Dr. Michael Markl: With 4D MRI, we’re actually able to measure the 3D blood flow in the heart and aorta of those patients. We then went on analyzing this data. What we actually found is that if we apply 4D flow MRI in patients at a certain point in time, we could identify a biomarker that would identify those patients who are at risk or at higher risk to developing aortic dilation and such complications at six to seven-year follow-up. This was a longitudinal study where we looked, can we measure something when the patient first presents at the hospital that would tell us more about their risk of complications later in life. We actually did find this new biomarker, and it’s called wall shear stress, aortic wall shear stress. It turns out if you have more of this wall shear stress in your aorta, you’re at higher risk for aortic dilation, which may eventually lead to the need for surgery and valve repair in those patients.
Adam Pick: I was curious to know if you could share a little bit more about the biomarker wall shear stress.
Dr. Michael Markl: Wall shear stress is actually a quantity that measures the drag force of the blood on the aortic wall. You can think of it like blood going through your aortic valve and if you have a bicuspid aortic valve, it’s a bit more narrow, so the flow is accelerated through that valve, and then it hits that aortic wall. Wall shear stress quantifies that force, and it’s actually been known for a long time the changes in shear stress can impact how the aortic wall remodels or gets more diseased. Then the higher the wall shear stress is, the more likely it is that you develop aortic complications. That’s exactly what we found in this story. What’s new here really is that for the first time, we were able to measure it in vivo in the patient with this novel imaging technique, 4D MRI.
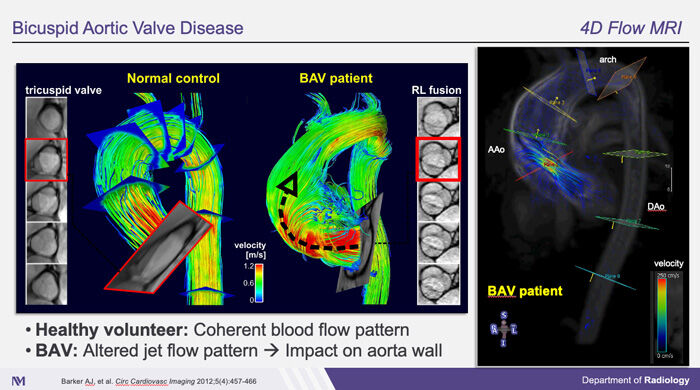
As you can see here, this actually shows the result of a 4D MRI scan in a healthy control on the left and a BAV patient in the middle. What you can actually see here is blood flow streamlines in the healthy control in the BAV patient and the color-coding here represents the blood flow velocity. Red means fast flow and green and yellow flow means slower flow. What you can actually really nicely see here, a healthy control has very cohesive, parallel streamlines that reflect normal blood flow whereas the BAV patient in the middle here has a very pronounced flow jet through the valve that hits the aortic wall. This is probably more evident if you look at the right, which is the same as in the middle but a video that shows the blood flow over time. You can very nicely see the development of this high blood flow velocity jet in red that hits the aortic wall. Again, the theory here is that with this new technique, we can visualize and measure these flow velocities. As you can see the jet hitting the wall, it’s an exact indication of the changes that happen in bicuspid aortic valve disease that can lead to aortic dilatation.
Adam Pick: With all this new, novel utility of 4D flow MRI, how is that going to help the heart team manage patients with bicuspid aortic valve disease?
Dr. Michael Markl: So we believe that with these new measures that we have wall shear stress and these new imaging techniques, I’ll have a much – potentially a much better method to define early on who might be at risk for developing complication. For the care team, that actually means if a patient comes to a hospital, they do this test, and early on in the life of this patient see there’s a higher risk of potentially developing this complication, they can adjust the management plan for that patient. They can say maybe this patient needs to come back for monitoring this every year, and we need to be very carefully monitoring the size of the aorta of that patient whereas somebody else may come in with normal wall shear stress. They may say well, you can come back in five years and we’ll check again.
It really is a tool to hopefully better manage patients and plan ahead for the remainder of their lives, pretty much. I mean, again, bicuspid aortic valve is a birth defect, so it’s something you carry with in your life, and you really want to plan ahead and manage that care as efficiently as possible for the patient.
Adam Pick: Michael, this is absolutely fantastic that you’re taking in innovation and making it a real-word, tangible utility for heart care teams to help their patients. On behalf of those patients, I want to thank you and the entire team there at Northwestern Medicine. Thank you so much.
Dr. Michael Markl: Well, thank you so much, Adam, for having me. It was really a pleasure to be with you and talk about our research. I’d also like to take this opportunity to thank our team. That’s actually very high cross-disciplinary and consists of physician engineers like me but we rely on the collaboration with cardiologists, cardiac surgeons, and other clinicians. I’d like to give a big thanks to everybody who had contributed to this research.





