Atrial Fibrillation & Heart Valve Disease: Top 13 Facts
Written By: Adam Pick, Patient Advocate, Author and Website Founder
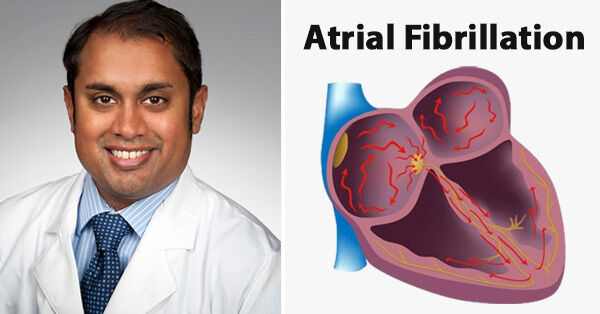
Medical Expert: Hemal Gada, MD, Interventional Cardiologist, UPMC Heart and Vascular Institute at UPMC Harrisburg
Published: May 12, 2022
We are getting lots of questions about atrial fibrillation and heart valve disease. For example, I just opened an email from Carole, an aortic valve patient, which reads, “Hi Adam, Do you ever talk about atrial fibrillation? I have it very bad. It seems like the Afib never lets up.”
To learn more about atrial fibrillation and heart valve disease, I was fortunate to connect with Dr. Hemal Gada, an interventional cardiologist and the medical director of the structural heart program of the UPMC Heart and Vascular Institute at UPMC Harrisburg. Dr. Gada previously completed fellowships at Cleveland Clinic for Cardiovascular Medicine and Columbia University for Interventional Cardiology and Structural Intervention.
1. What is atrial fibrillation?
Atrial fibrillation, or A-fib, is the most commonly treated arrhythmia, or heart rhythm problem. The CDC estimates that more than 12 million people in the U.S. will have AFib by 2030. It’s a serious condition because left untreated, it increases your risk of blood clots, heart failure, and stroke. A-fib is when the upper chambers of your heart (atria) beat out of sync with the lower chambers (ventricles).
 (Source: Centers for Disease Control & Prevention)
(Source: Centers for Disease Control & Prevention)
2. Is A-fib preventable?
Preventative measures to reduce the risk of A-fib include taking simple steps against risk for coronary artery disease or high blood pressure. Basic lifestyle habits that could significantly reduce the risk of developing A-fib include not smoking, following a heart-healthy Mediterranean-style diet (high in plant-based foods, fruits and vegetables, and low in saturated fats), being physically active, and managing your weight.
There’s a lot you can do to prevent and control A-fib, but when it is caused by a heart valve issue, surgical intervention may be required. A-fib can sometimes develop following heart surgery to fix a non-related condition. If this occurs, it will need to be monitored and treated and is commonly referred to as post-operative A-fib.
3. What are some symptoms that are related to AFib that I should watch for?
Whether you have non-valvular or valvular A-fib, the symptoms are often the same. The main symptom is feeling like your heart is fluttering, racing, or thumping. Other symptoms can include:
- Chest pain or pressure.
- Dizziness or lightheadedness.
- Excessive tiredness or weakness.
- Faintness or confusion.
- Fatigue when exercising.
- Heart racing when sitting still.
- Shortness of breath and anxiety.
- Sweating.
4. How does a doctor diagnose A-fib?
An electrocardiogram (EKG) is commonly utilized to diagnose A-fib. It is a test that measures the electrical activity of the heartbeat. With each beat, an electrical impulse (or “wave”) travels through the heart. This wave causes the muscle to squeeze and pump blood from the heart. A normal heartbeat on EKG will show the timing of the top and lower chambers.
In this test, a doctor can determine how long the electrical wave takes to pass through the heart. Finding out how long a wave takes to travel from one part of the heart to the next shows if the electrical activity is normal or slow, fast or irregular.
5. Am I at risk for other heart conditions as complications from A-fib?
A-fib increases your risk of blood clots, heart failure, and stroke. In general, A-fib causes some 158,000 deaths in the U.S. each year.
If you have valvular A-fib, you’re at an even greater risk of blood clots than those who have non-valvular A-fib. That’s because having mitral valve stenosis or an artificial heart valve already increases your risk of blood clots.
6. Is my A-fib the same as my coworker or family member that also has A-fib?
In general, there are two types of A-fib. Non-valvular A-fib is the kind you can control with lifestyle changes and medication. Risk factors for developing non-valvular A-fib include high blood pressure, diabetes, obesity, smoking, heavy drinking, and chronic stress.
Valvular A-fib, on the other hand, is related to valvular heart problems, such as mitral valve stenosis or having an artificial heart valve. An estimated 4-30% of people with A-fib have valvular A-fib. It’s a wide range because doctors don’t agree on when heart valve problems are the cause of A-fib.
7. If I’ve been diagnosed with AFib, what are my options to manage my condition?
If you have A-fib, it’s important to get treatment. Treatment options include medication, surgery, and outpatient procedures.
8. Can I use medication to manage my A-Fib?
Medications are often used to manage A-fib. When talking to your provider, some different medicines mentioned may include:
- Anticoagulants and antiplatelets. Atrial fibrillation increases your risk of blood clots. So, it’s often treated with blood thinners and similar medications that keep your blood from clotting.
- Medications to slow and control your heart rate. Most people feel better once their heart rate resets. These medications include beta blockers, calcium channel blockers, and digoxin.
- Medications to control your heart rhythm. If you need additional medications to control your A-fib, your doctor can use an anti-arrhythmic drug. These include sodium channel blockers and potassium channel blockers.
9. Is surgery always my next step if medicine doesn’t manage my heart’s rhythm?
If medications don’t work or you can’t take them, there are other options, these include:
- Electrical cardioversion. For this outpatient procedure, doctors use a machine to deliver a low-voltage electric current to your heart. This can help restore your heart’s normal rhythm.
- Catheter ablation. This minimally-invasive procedure attempts to isolate the tiny parts of your heart that are sending abnormal electrical impulses and causing A-fib. Doctors insert thin wires called catheters through a vein up into the heart. Electrodes at the end of the wire deliver heat, which can destroy the tissue causing the A-fib.
- Surgical ablation. For this option, also called the MAZE procedure, surgeons create scar tissue with small incisions, radio waves, freezing, or microwave or ultrasound energy. The scar tissue blocks the abnormal electrical signals that cause A-fib.
- Left atrial appendage closure. This procedure lowers your risk of stroke. A surgeon implants a device known as the WATCHMAN™ into your heart to close off the part of the heart that most commonly forms stroke-causing clots.
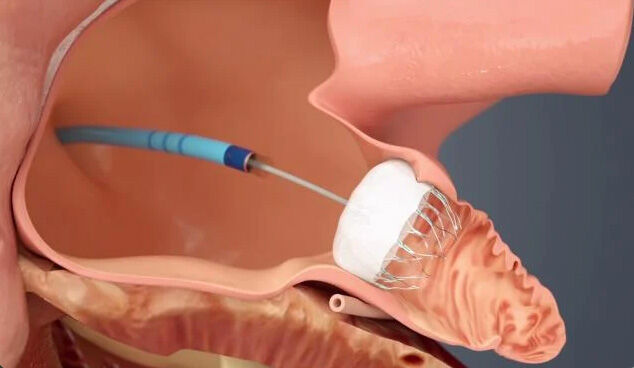 The WATCHMAN (Source: Boston Scientific)
The WATCHMAN (Source: Boston Scientific)
- Implanted devices. A surgeon puts a device, like a pacemaker or an implantable cardioverter defibrillator (ICD), in your heart to monitor your heart’s rhythm. If they detect abnormal rhythm, they deliver an electric shock to restore normal rhythm.
10. How can heart valve surgery correct my Atrial Fibrillation?
For those with valvular A-fib caused by a faulty aortic or mitral valve, heart valve surgery can repair or replace damaged heart valves. Your surgeon can often also work to correct A-fib during surgery for other heart issues. However, even after having heart valve surgery, it not uncommon to still have A-fib.
According to the American Heart Association, A-fib is the most common complication after heart surgery. A-fib after heart valve surgery increases your risk of heart failure and dangerous blood clots known as thrombo-embolisms.
When heart valve surgery doesn’t fix your A-fib but addresses major valvular deficiencies in your heart, your doctor can consider other surgical options.
11. Can aortic valve replacement cause A-fib?
After open heart surgery, a third to half of all patients develop A-fib. Several types of open heart surgery can trigger A-fib. This includes aortic valve replacement, where your surgeon replaces a narrowed or leaky aortic valve.
Other types of open heart surgery that can trigger A-fib include:
- Coronary bypass surgery.
- Heart transplant.
- Mitral valve repair or replacement. Your surgeon will either repair or replace a leaky or narrowed mitral valve.
12. What are some common risk factors that could lead to developing A-fib following a heart surgery?
It’s unclear why someone develops A-fib after open heart surgery, but risk factors include:
- An electrolyte imbalance after surgery.
- Chronic obstructive pulmonary disease (COPD).
- Genetic predisposition for A-fib.
- Heart failure.
- High blood pressure.
- Obesity.
- Older age.
- Pneumonia after surgery.
- Surgery on a heart valve, such repair or replacement of aortic valve or mitral valve.
- Thyroid problems.
13. How serious is A-fib after heart surgery?
Developing A-fib after heart surgery leads to longer hospital recovery, more time in intensive care, and worse long-term outcomes. Along with the usual increased risk of stroke and heart failure, A-fib after surgery can increase your risk of infection, kidney dysfunction, and brain dysfunction.
A-fib typically develops within seven days after open heart surgery, but it can also take up to 90 days to notice A-fib symptoms.
In some cases, A-fib is temporary, only lasting a few days. Then it goes away on its own. For others, A-fib after heart surgery is permanent and doesn’t go away. In this case, you’ll need to receive treatment for the condition.
Many thanks to Dr. Gada and the UPMC Heart and Vascular Institute!
On behalf of our community, many thanks to Dr. Hemal Gada for sharing his clinical experiences and research with our patients. We also want to thank the entire UPMC Heart and Vascular team for taking such great care of heart valve and atrial fibrillation patients.
Keep on tickin!
Adam





