Surgeon Q&A: “What Determines the Transfemoral or Transapical Approach for TAVR?” Asks Denise
By Adam Pick on September 18, 2013
Given the recent FDA approval of transcateher aortic valve replacement devices (TAVR), I continue to receive interesting questions from our patient community. For example, Denise recently wrote to me, “Hi Adam – My mom is 84 years old and diagnosed with severe aortic stenosis. We’re researching the possibility of using the catheter valve to help her. I’ve read that the valve can be inserted through the groin or through the heart. What determines the way in which this valve is implanted? Is one better than the other? Thanks, Denise.”
Denise raises a great question. That said, I wanted to provide Denise a great answer. For that reason, I contacted Dr. Mathew Williams, at NYU Langone Health. So you know, Dr. Williams is uniquely qualified to address Denise’s question considering that he trained in both cardiac surgery and interventional catheter-based techniques.
About the Transfemoral and Transapical Approaches for TAVR
In his response to Denise, Dr. Williams made several helpful distinctions about TAVR and the transfemoral and transapical approaches. He also referenced the transaortic approach which I was unfamiliar with.
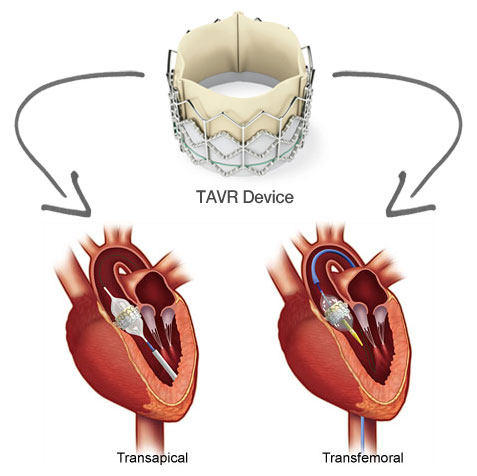
Hello Denise, thank you for your question. Transcatheter Aortic Valve Replacement (TAVR) is a viable treatment option for patients who are diagnosed with severe aortic stenosis and are high risk for open heart surgery due to their age or other medical conditions making them poor candidates for surgery. Approximately 80 percent of our patients have the procedure done through the femoral artery, or a transfemoral approach. A catheter is placed in the groin area and a new valve enclosed in a metal stent is threaded to the diseased aortic valve using the patient’s vessels as a pathway. The prosthetic valve is carefully positioned, expanded, and anchored inside the diseased valve. The transapical approach is designed for patients who have small or diseased vessels preventing access from the groin to the aortic valve. A small incision is made just under the left chest and the valve is advanced through the ribs to the apex, or tip of the heart. A third approach is currently in clinical trials, called the transaortic approach. The transaortic approach involves direct access to the aorta through a small incision on the top portion of the breast bone. This is also designed for patients who have inadequate femoral arteries. Your mother will have several diagnostic tests before her procedure to determine which access route is best for her.

Dr. Williams then addressed the preferential technique for TAVR procedures:
Our preference is to use the transfemoral approach when possible because the recovery time in the hospital is shorter. Patients who have a procedure done via the transfemoral approach on average recover in the hospital for three-five days barring any complications. Those who have the transaortic or the transapical approach can expect to remain in the hospital between five-seven days to ensure the incision heals properly.
Finally, Dr. Williams addressed Denise’s patient advocacy efforts and the need for action specific to aortic stenosis:
The great news is that you are exploring treatment options for your mother. Aortic stenosis is a very aggressive disease and the two year survival rate for symptomatic aortic stenosis is less than 50% if left untreated. Whether your mother has surgery which is also an excellent therapy with very positive outcomes, or TAVR, we encourage your mother to seek treatment earlier rather than later for the best results. Good luck and I hope your mother’s treatment is a success. — Mathew R. Williams, MD
I hope this helped you learn more about the transfemoral and transapical approaches for TAVR. Thanks to Denise for sending me this question and a special thanks to Dr. Mathew Williams for sharing his clinical experience and research with our patient community!
Keep on tickin!
Adam
|
Renata Cimões says on September 18th, 2013 at 5:49 pm |
|
Dear Adam, I have a lot of questions about this procedure TAVR. Is this approach possible to children? My son is 1 year, and he has aortic stenosis. Your web site is helping me a lot. |
 |
|
Jens says on September 25th, 2013 at 3:08 pm |
|
Hi Adam, I had surgery two and a half years ago and had, at the age of 46, my aortic valve replaced with a biological valve. Knowing that I will at some time in the future be in need for a second surgery, one question always springs to mind, when I read about TAVR: Can I within my time span expect devices or techniques to develop in a way where the approach will be recommended to not only high-risk patients? How do experts see the developments, and what do they expect? Yours sincerly, Jens |
 |
|
Richard Holoubek says on September 25th, 2013 at 5:59 pm |
|
I had my aortic valve replaced 4 years ago with a bovine valve. I am very healthy now however I was told it may last approx. 10 years or longer. If/ when it needs to be replaced… Is TVAR an option? My specific concern is whether the non-tissue structure of the bovine replacement won’t allow a TVAR replacement option? Any ideas about my concern? |
 |
|
Doris Holloway says on October 20th, 2015 at 3:08 pm |
|
Is the TAVR procedure available for aortic regurgitation? I’m not seeing any mention of it. |
 |
|
James Richards says on July 17th, 2018 at 11:01 am |
|
I had TAVAR procedure except they opened my chest with about a 4 inch incision and separated the sternum. Have a swine valve inserted this was last November, I had infection occur and complications after the surgery and am still in recovery. I am 72 years old and have diabetes. What could cause the bones to not heal such I have read in these and other de |
 |