“Are Pleural Effusions Common After Heart Valve Surgery?” Asks Jan
By Adam Pick on October 10, 2009
Jan just sent me an interesting email about pleural effusions and heart valve surgery.
In her note, Jan writes, “Dear Adam, I am the caregiver of my 59-year old brother who had aortic valve replacement (with a bovine valve) at Vanderbilt University Hospital on July 13, 2009. The valve itself has done okay but he has been in-and-out of the hospital twice since surgery. Fluid continues to collect between his chest wall and right lung. The fluid has been drained twice. Is this common? Thanks, Jan”
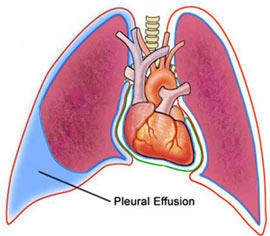
It sounds to me like Jan’s brother is experiencing a post-operative complication known as a pleural effusion.
According to The Cleveland Clinic, a pleural effusion, sometimes referred to as “water on the lungs,” is the build-up of excess fluid between the layers of the pleura outside the lungs. The pleura are thin membranes that line the lungs and the inside of the chest cavity and act to lubricate and facilitate breathing.
The common symptoms of pleural effusions after heart valve surgery are:
- Chest pain
- Dry, nonproductive cough
- Dyspnea (shortness of breath, or difficult, labored breathing)
- Orthopnea (the inability to breathe easily unless the person is sitting up straight or standing erect)
Specific to Jan’s question, “Are pleural effusions common after heart valve surgery?”, there are about 100,000 total cases diagnosed in the United States each year, according to the National Cancer Institute.
During my research, I learned that pleural effusions are somewhat common after cardiac surgery. Net Wellness suggests, “Post-operative pleural effusions are common in patients who undergo cardiac surgery. Most of these effusions develop as a consequence of the surgical procedure itself and follow a generally benign course.”
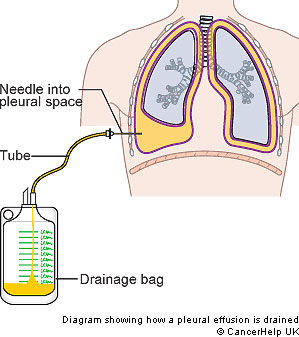
Specific to the use of drains to clear the pleural effusions… Karen Kutoloski, Director of the Cardiac Rehabilitation and Assistant Professor at MetroHealth Medical Center, suggests that while pleural effusions can be relatively common, post-operative chest tube drainage is rarely required. Accoring to Kutoloski, most pleural effusions are small and asymptomatic.
- Related Post: Pleural Effusions & Heart Surgery: 7 Important Facts
I hope this helps answer Jan’s question about fluid in the lungs after heart valve replacement and heart valve repair procedures. Unfortunately, it sounds like Jan’s brother falls into a relatively small category of patients that required fluid drainage after heart valve surgery.
Keep on tickin!
Adam
|
Tony Korwin says on October 10th, 2009 at 1:47 pm |
|
I too, experienced a pleural effusion after mechanical valve replacement.. My surgeons colleaque would come in the morning and tell me I was not using the spirometer enough and they were worried about pneumonia.. about 5 days after surgery, they finally called in a lung specialist and after a quick ultrasound, pronounced I had fluid on the lung. It turned out to be blood, not water.. over 1 liter had completely collapsed my left lung. He stated it was a fairly rare event that would not repeat and thus far he is correct. Once they drained the blood, I could finally breath a decent breath in the sprirometer. |
 |
|
Kerrigan says on October 10th, 2009 at 2:07 pm |
|
I had fluid building up in my abdomen to the point of bloating, taught skin, and discomfort. They put me on a mild duretic and the problem subsided. |
 |
|
Mary Campbell says on October 10th, 2009 at 2:24 pm |
|
Hi, I had descending aortic valve and aneurysm repair on December 2, 2008 at the Cleveland Clinic. I returned to my home in Arizona and was feeling great upon my return, but shortly after New Years, I developed extreme pain in my left shoulder and under my rib cage. I could not get up from my recliner and no matter what I did the pain would not go away. I awoke at 3 a.m. thinking I was having a heart attack. I immediately called for help and was taken to the hospital near my home, It was determined that I had pleural effusion and the new cardiologist attending me wanted to drain the fluid. I explained that the fluid was around my heart when I was discharged from the Cleveland Clinic. I also asked that they call and request my surgical history. The cardiologiist in Cleveland told the cardiologist in Arizona what type of medication to place me on, which is normally given to Gout Patients but which also helped me to got rid of the fluid fairly quick. I felt 100% better within just a few days. I can surely understand how scared pleural effusion is to a patient and caregiver, but as it was mentioned by Adam, it’s very common after heart surgery and usually goes away by itself. |
 |
|
Nancy says on October 10th, 2009 at 4:26 pm |
|
I developed both pleural effusion and effusion around the heart. Both were drained and I felt much better. |
 |
|
Jim Cummings says on October 10th, 2009 at 6:48 pm |
|
One week after surgery to replace my aortic valve, I developed cardiac tamponade. A pericardial procedure was done to drain over a liter of fluid from around my heart. My understanding is that an effusion can develop into tamponade. I remember doing a lot of breathing treatments and other excercises to keep fluid from building up on my lungs. |
 |
|
Keith Ebden says on October 10th, 2009 at 7:17 pm |
|
I too had a left pleural effusion after about 10 days. I had been recovering very well and it was like I had hit the wall. I had 800ml drained to no effect and diuretics which also did nothing. After a frustrating week I saw my surgeon who said I should ignore the previous advice to take things easy and really push the exercise until I was well out of breath – it cleared up within a few days! |
 |
|
Shelley says on October 10th, 2009 at 8:35 pm |
|
My experience was very similar to one of your other responders. I had aortic valve replacement (bovine) on a Tuesday morning. In recovery the doctor explained that they almost had to take me back to surgery for excessive bleeding. After a transfusion they finally got the bleeding to stop. On Wednesday they gave me another transfusion. They were concerned that I still required some oxygen by Saturday night so a pulmonary doctor did a sonogram and said my right lung was collapsed due to fluid. He did a thoracentesis and removed 1 liter of blood. I was off all oxygen by the next afternoon and discharged on Monday. |
 |
|
Nancy Scharf says on October 11th, 2009 at 1:44 am |
|
I also experienced a pleural effusion after mitral valve replacement in July or 2000. I was readmitted to the hospital, a drainage tube inserted and stayed for a week while draining litre upon litre of fluid. The fluid added 35 to 40 pounds of very uncomfortabel weight. Fortunately I left the hospital and my cardiologist took over my care and eliminated that problem along with other complications. This is the first I’ve heard that this is pretty common after the surgery. I have aortic stenosis now and hope I will not need another replacement. Isn’t there some way to prevent the chance of a pleural effusion? |
 |
|
greg says on October 11th, 2009 at 9:59 am |
|
4 weeks after my triple bypass on sept 1 they removed a quart from my chest cavity. thinking I had pneumonia they kept me in hospital for three days and then sent me home. they tried to culture the fluid but no bacteria materialized. for three days they loaded me with cypro anf other anibiotics. the thirty something doctor was convinced I had pneumonia no matter the lab results. I was saved by my cardiologist who intervened and basically told the other doctor that this was normal for heart patients. it has been a month sice this happened and the fever has not returned and I have a small amount of fluid around my left lung. I was told this may or may not go away. |
 |
|
Janet Coyle says on October 11th, 2009 at 4:26 pm |
|
I had a bovine aortic replacement at the Cleveland Clinic on October 30,2009 and returned to my home in Florida about 1 week later. I developed a severe cough and was hospitalized for a large pleural effusion and underwent a thorosentesis which drained about 1 liter of fluid with blood, Between mid November and mid Dec. I had 2 more pleural effusions which were draided on an out patient basis. Each procedure drained less and I have had no further prolems with this since De. I was told that pleural effussions are commom post aortic replacement and occurs at some level in >60% of patients. I was told that this hyper fluid response is caused by the lungs being deflated during the surgery and can sometimes recur up to 1 year post surgery. |
 |
|
susan spagnola says on October 12th, 2009 at 7:44 pm |
|
I was just reviewing my medical records from surgery to repair my mitral valve two months ago. I was startled to see a report of “bilateral pleural effusion” and a bit relieved that it appears to be somewhat common after heart surgery. I have no symptoms that seem to be consistent with pleural effusion, but will follow up with my cardiologist to make sure that this is nothing that I need to have monitored. |
 |
|
Will Ford says on October 12th, 2009 at 9:02 pm |
|
I had aortic valve relacement surgery in November, 2008. Surgery and recovery were successful and quite uneventful EXCEPT for recurring pleural effusion and 3 thorocentesis (drainage) procedures. I have significant shortness of breath upon stair-climbing, walking any distance or exerting most physical activity. Pulmonologist is still trying to come up with some beneficial treatment. A definite downer that no one mentions PRIOR to surgery. |
 |
|
Cheryl says on October 14th, 2009 at 8:42 pm |
|
Hi Adam I asked my family physician today to double check on my right lung and she couldn’t really understand why I was asking. I’m going to monitor how I feel myself and perhaps tomorrow if I can’t definitely see improvement, will insist she see me. I’d rather be safe than sorry. Perhaps I’m not explaining the symptoms correctly but I know that is what is noted on my discharge papers including the request for family physician follow-up and x-ray. I don’t mind discomfort but I would worry if there were any dangers involved that I should be aware of. |
 |
|
James Nagy says on October 18th, 2009 at 6:06 pm |
|
Adam, |
 |
|
sharon says on November 2nd, 2009 at 1:39 pm |
|
Adam, I had plureal effusion after my aorta valve replacement in Feb. 2009. I had a lot of difficulty breathing and severe pain in my back shoulder blade area on the right and a cough I could not shake. The home nurse diagnosed it before any of my drs. agreed finally. Once the chest x-ray came back I had to go and have the effusion drained, which was relatively painless and fast to my surprise and relief. |
 |
|
Terry Hardcastle says on November 8th, 2009 at 12:44 pm |
|
hi, ive just two months ago underwent bypass surgery to repair two blocked arteries, two weeks afte released from the hospital, i had to go in and have fluid drained from both lungs,,,there was close to a qt. of fuild in each side,,,i felt so much releaf, then two weeks later i had to go again,,,not as much fluid in the right lung but still close to a qt on the left lung,,,now this is three weeks after the last time and ive got to go in and have the fluid drained again,,,they told me friday that i only had the left side with fluid, the right has none…im wondering if this will stop or am i in for this every two or three weeks… |
 |
|
Denise Dudum says on November 21st, 2009 at 7:11 pm |
|
I had a very sucessful mitro valvue repair 30 days ago and have developed plureal effusion. I have already been drained 3 times. This is an extremely painful experience. |
 |
|
paulette gosnell says on March 9th, 2010 at 11:06 am |
|
I had mitral value repair 6-29-09,and had 3 pleural effusions,afterwards,my surgeon explained to me,was probably due to my small stature.95 lbs.5’3″,he expected me to have some complications going in,however I was not prepared,for everything that I had to go through ad 58 years old. |
 |
|
Mary Keefer says on April 9th, 2010 at 11:58 am |
|
I am 11 weeks post mitral valve repair; about 15 days postop developed plural effusion. Went to ER due to pain level and was admitted for 3 days on medicine therapy (no aspiration). Dr. has since treated with Colchicine (gaut RX also used for this problem), ibuprofen 600 mg daily and finally a diminishing dose of Prednisone. Very discouraging, as it returned about a week after the Prednisone was completed. Am headed back to the doctor ths morning. Hope I don’t end up back in the hospital! |
 |
|
wayne sykes says on April 21st, 2010 at 4:43 pm |
|
I have post operative infusion and returned to the hospital a week after going home with extreme pain and inability to breath. For 3 days I was very frustrated because I felt no one was taking my pain seriosly. It was not until I started running a fever that they began action. I also felt like no one was giving me any answers. I went for a tap to remove some fluid to make sure it is not a bacterial infection but there was not enough to withdraw safely. I wish that more had been done to educate me and my family about this possible complication since it seems to be fairly comon. We would not have so worried and scared. |
 |
|
Verna says on June 8th, 2010 at 6:44 am |
|
I had double coronary artery bypass surgery five weeks ago. I am experiencing some pleural effusion. Have been on lasix 20 every day but it doesn’t seem to be helping much. This morning I awoke with pain under my left breast and to the left that increased with deep breaths. The pain went away when I stood up. I am an RN so listened with my stethoscope and can hear a definite friction rub. I know these are usually benign and eventually reabsorb, but this is worse than before which concerns me. I had an echocardiogram done yesterday but didn’t have the pain then, so don’t know if it showed or not. I see the Dr. tomorrow. Should I wait and see or call him now? |
 |
|
Michelle says on August 14th, 2010 at 1:21 am |
|
Im almost 3 weeks post op for mitral valve repair. Three days ago I went to the ER for sharp pains under my right lung and a fever. I have 500 cc of fluid on my right lung and just a little on my left. It was very frustrating because I felt like I was slowly recovering and then all of a sudden I felt as bad as post op day 2. They put me on motrin 600 mg twice a day and zpack antibiotics. I was told that walking, avoiding sodium and drinking tons of water will help clear it. So far the pain is almost gone but lying down my lung still feels gurgley and my temp has been up to 99.6 once in a while. I hope it goes away soon. I also found out I’m anemic. I didn’t mentally prepare for the after math of surgery like I did for the surgery itself so I feel emotionally more vulnerable to these set backs. |
 |
|
K.C.Mittal says on August 22nd, 2010 at 7:22 am |
|
My wife aged 72 years went into surgery for the replacement of aortic valve in a DELHI hospital, in August 2008. After about 30 days she was detected having pleural effusion of the pericardium and lungs. She was taken back to the same hospital. Pericardial effusion was removed by a special catheter, and it was about 800 grama, it was something like puss It did not stop and carried on slowly. The pleural effusion was not removed. The doctors prescribed certain medicines, and discharged her, and declared she had some infection pericardial effusion did not stop so a window was opened , she could not recover and died after 20 days due to sepsis and DIC. She was given a lot of blood and platelets transfusions. I believe she died due to unavailability of the required treatment. What do you say? |
 |
|
Chris says on August 22nd, 2010 at 5:51 pm |
|
I had my aortic valve replaced with a bovine valve Jan. 2005. I had a pleural effusion in my right lung post surgery and had some difficulty with pain and breathing for a few days. I was given a diaretic and got rid of the fluid naturally in two days. I did not need to have it drained. |
 |
|
Bill says on November 2nd, 2010 at 12:18 pm |
|
Hi Adam, P.S. We appreciate your book. |
 |
|
Karen says on November 15th, 2010 at 4:47 pm |
|
My mum has recently had aortic valve replacement 3 days ago, she is out of ITU today whith breathing difficulties, a chest xray today showed fluid on the lung. A few days ago while in ITU she had problems breathing and was told that her right lung had deflated. She is also very hot and sweaty and cannot complete a sentence as she is so breathless, she is currently on 4 litres of oxygen. What is her prognoses of recovering? |
 |
|
swamy says on December 4th, 2010 at 5:09 pm |
|
My father underwent triple bypass with Mitral Valve Replacement in October. He has since been drained twice(both within a fortnight of the surgery) and has since been asymptomatic though the most recent xray still shows pleural effusion. Fingers crossed on how things are going to unfold. |
 |
|
Donna says on March 6th, 2011 at 3:02 pm |
|
On May 20th 2010, I had a mechanical aortic valve replacement, my mitral valve repaired & one bypass. I went home one week later. I returned to the hospital the following July & had to have chest tubes in both sides> They drained a total of 2500 ml from both lungs> I am now at home with Pluerx chest tubes that i have to drain at least once a day. I get anywhere from 600 to 1200 ml off each side daily! The doctors say this could go on for a year! Thanks to everyone for sharing your stories! I don’t feel so alone now! |
 |
|
Fran Zilko says on March 7th, 2011 at 4:33 pm |
|
Hi Donna |
 |
|
Danni says on June 23rd, 2011 at 2:37 pm |
|
Hello all, I am a 28 year old female and I underwent open heart surgery on March 14, 2011 at UCSF. I had my aortic valve replaced with a bovine valve. I used my incentive spirometer more than most patients according to the nursing staff and I even took it home and used it for weeks in fear of lung complications. I too experienced a pleural effusion after surgery in my 3rd week post op. I was having difficulty breathing and an old rib injury was really flaring up because of it. I didn’t know what it was until they took an x-ray and found the fluid. They sent me home with a diuretic and potassium pills to dilute the water retaining sodium. I took those and drank little water for a week and dehydration pulled the fluid out. No drain tubes. It reocurred in my 5th week post op, so I called in to get more diuretic and potassium pills. This time it cleared up in around 3 days from pure dehydration. I guess when dehydrated other areas of your body need the fluid so it pulls it right out. I was told to stay hydrated after surgery, so I was surprised of this treatment but it worked and was way better than tubes 🙂 Hope this helps!! |
 |
|
Linda says on August 21st, 2011 at 2:18 pm |
|
Hello, |
 |
|
Nancy Trojanowski says on January 9th, 2012 at 5:43 pm |
|
My mom had her aortic valve replaced in October 2011 and has had two pleural effusions with thoracentesis. They have now placed a pleurx catheter in her which we will drain at home. Has anyone had any experience with this complication following open heart surgery. |
 |
|
Nancy Tankersley says on March 17th, 2012 at 6:29 pm |
|
I had mitral valve repair Feb 2 2012. On the 4 th day my drainage tubes were removed and I began to bleed internally. On Feb 7 I had a second surgery where they discovered a tear or cut on my left mammary artery. At least two pints of blood were removed. Four days later a large pleural effusion was discovered around my left lung and a drain was inserted in my left side. I remained in the hospital until Feb 28 when it was finally determined that the amount of fluid was small enough to finally send me home without a diuretic or a drain. My breathing did not improve at home nor did the effusion shrink so now I am back on LASIK and feeling better. After reading all of the comments I am going to try to increase my activity in the hopes the effusion will shrink. My cardiologist doesn’t seem worried and told me to go ahead and plan for an out of county trip in September. I’m a bit worried that the effusion , after it does go away,will return. I’m a 62 year old female and this is my second repair. The repair itself seems to have been very successful although I still,have a small amount of atrial fib so am on Coumadin. My cardiologist is optimistic the atrial fib will go away. |
 |
|
Linda Aldrich says on March 18th, 2012 at 10:29 am |
|
I had mitral valve repair September 2009. The surgery went well. Months before when I had my cath I was given an aspirin 325 mg. and broke out in a rash. After surgery they gave me an aspirin 81mg against my better judgement saying the benefits were best for me. Well, I broke out in a full blown, head to toe rash with fever and terrible itching. They could not treat the rash until they determined that there was no infection in my heart. So after days of cultures, pic line, dermatology consults, I laid there and itched. I ended up being in the hospital for 11 days! Most of that time I laid there and itched while my heart healed. My cardiologist would say “your heart is healing fine it is just this rash” |
 |
|
Nancy Welch says on March 21st, 2012 at 7:35 pm |
|
I had pleural effusion that needed to be drained. Immediately I breathed better. Sometimes it needs to be drained more than once. |
 |
|
Mary says on July 24th, 2012 at 3:34 pm |
|
I had aortic valve replacement and mitral valve repair a year ago (July 2011). I was home for a week, and returned to the hospital by my cardiologist for treatment of pleural effusions. After 3 thoracentesis procedures and the removal of 3.5 L of fluid, I wish I could say that I was “cured.” I have continued to take diuretics all year in hope of resolving the remaining small pleural effusions. This month the situation blew up on my left side, and I had 800 ml of fluid removed in another thoracentesis procedure, which resulted in a collapsed lung (pneumothorax). This was treated, but the effusion has returned and is occupying about 1/2 of the chest space on my left side, resulting in breathing difficulties. I am of average weight and I do not have congestive heart failure; these effusions are a side effect of the valve surgery. I am seeing a thoracic surgeon next week to discuss surgical procedures to resolve these effusions (thoracoscopy or thoracotomy). Has anyone gone through anything like this? I’m getting desperate to resolve this situation! |
 |
|
Linda Johnson says on September 17th, 2012 at 5:29 pm |
|
I had aortic valve replacement and tricuspid valve repair on August 1. I was doing fine when I hit what others have described as a wall, caused by pleural effusion. I had 600 ml of fluid drained on August 1 and 825 ml on September 10. The relief is instant but doesn’t last, as I am once again breathless upon mild exertion. I see my cardiologist on Friday to find out what’s what. Glad to know I’m not alone! |
 |
|
Bill says on November 30th, 2012 at 1:43 pm |
|
My 87 year old mother had open heart aortic valve replacement surgery @ washington Hospital Center. Now after several weeks of relapses in Georgetown it appears that fluid build up in the lungs could be the culprit. She was relatively healthy for a 87 year old but with complications from shortness of breath and irregular heart beat she is fighting a courageous up hill battle. What can I tell her for any reassurance ? Hang in there? I feel better having read comments from other patients.. |
 |
|
David Driscoll says on February 25th, 2013 at 4:32 pm |
|
my 84 year old mother-in-law is 4 days post-op for mitral valve replacement and the resection of a dissecting anneursym of the aortic arch. She seems to be recovering well but for a pleural effusion that is currently being treated with Lasix for pleura l effusion |
 |
|
Elizabeth Concepcion says on March 21st, 2013 at 1:04 am |
|
My mother had mitral and tricucspid valve repair and PDA ligation! She developed bilateral pleural effusion! She had right pleural effusion preop and had thorax enteric twice before undergoing surgery! Post op she developed bilateral effusion worst on the left lung that requires initially aspiration of bloody drainage( INR was elevated at around 8) that’s what the surgeon had explained why its bloody! After 2 days post aspiration, pleural fluid built up again and now she has a Blake more tube connected to JP drain to her left chest! Right lung pleural effusion resolve on its own!The 2 d echo post op shows mitral and tricuspid valves are working ! She has the left blakemore tube on her left lung for a week now and continue to drain at least 300 cc for 24 hours! Need your opinion on what’s going on! Thanks |
 |
|
mansoor says on March 30th, 2013 at 4:22 am |
|
why pleural effusion post heart valvular surgery occurrence frequently although treated with pleural tap or drainage? |
 |
|
Walter Godinez says on April 16th, 2014 at 9:58 pm |
|
I had aortic valve replacement (mechanical valve), and an ascending aneurysm graph in Jan. 2014, Recovery was going fine but last week 04/10/2014 I developed a productive cough I could not shake it and a fever ensued, went over to my regular doctor and she prescribed some antibiotics and sent me over to check my INR because of my Coumadin and while I was there she order a chess x-ray stat! I went home after picking up prescriptions at the local pharmacy. After a couple of hours she gave me a call and inform me that she could not make it out, but there was ether an enlargement of the heart or fluid buildup in the pericardial cavity! She sent me to the ER and after an echo cardiogram it was confirm that there was a substantial amount of liquid in my heart cavity! I did have the pericardial cavity drained of over a litter of liquid and they put another chest tube in. I was in the hospital for another 3 more days. Now the matter is getting my Coumadin levels back to 2-3 INR and hope that this does not happen again. My fever is gone I can breathe much better but I still have that horrible cough, hopefully it goes away in couple of days then maybe I can enjoy my life and family once again! |
 |
|
June says on April 22nd, 2014 at 7:59 am |
|
I had open heart surgery in Sept. 2013, and I just had my pleura effused Fri. April 18,2014. They look a liter out and my lung was partially collapsed due to this fluid. I still don’t feel any better, just pain from the effusion. |
 |
|
Diedre says on July 25th, 2014 at 1:26 am |
|
It seems there is a lot of pleural effusion despite this doctor’s blog that says it is rare. Interesting – comment after comment after comment, yet it’s rare! My Mom is currently 2 weeks post op for a valve replacement and all signs indicate pleural effusion, yet the post-op doctors and rehab people aren’t calling it that. I am hoping they will diagnose that, drain it before she has to leave rehab for home. The fluid doesn’t seem to be leaving, first it was edema, now shortness of breath a day or so later, which upon reading all tehse comments sounds like this pleural effusion. |
 |
|
M A says on August 8th, 2014 at 1:20 pm |
|
Dear Adam, Thanks |
 |
|
Michelle Keplinger Larsh says on January 7th, 2016 at 11:30 am |
|
Thank you for taking the time to post this! Every post helps me to better understand what might be going on with my Dad! Thank you again! |
 |
|
Mark Eicholtz says on December 27th, 2016 at 9:40 pm |
|
“Most of these effusions develop as a consequence of the surgical procedure itself and follow a generally benign course.” … what does “a consequence of the surgical procedure itself” mean ? Please elaborate. |
 |
|
Lynne Newcomer says on April 27th, 2017 at 5:51 pm |
|
I am 2 months post open heart, I had a repair of the mitral and tricuspid valves, septal myectomy ,double by pass, and a atrial clip……I was told I had a bit of fluid around my left lung, by was advised that it would resolve its self. I continue to have shortness of breath along with extreme weakness intermittently … will this pass ? |
 |
|
Jen says on July 24th, 2018 at 11:59 pm |
|
How are you now? My mom is in this situation draining at home |
 |